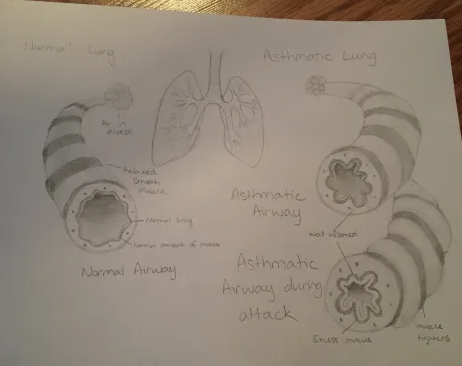
My project is on the role asthma plays in respiratory dysfunction. It looks at how our respiratory system is altered with each asthma attack. It then takes a brief look at intervention/management of asthma. My project covers course the course objective “Analyze the effects of disease on function and structure of the respiratory system.” The basic idea of my art was to show the difference between a normal lung and an asthmatic lung, highlighting just how asthma affects the respiratory structures.
Asthma, a prevalent chronic respiratory condition, affects more than 300 million people worldwide (Habib et al., 2022). This complex disorder, characterized by chronic inflammation and airway hyperresponsiveness, leads to recurrent episodes of wheezing, breathlessness, chest tightness, and coughing (Habib et al., 2022). It’s a condition that knows no boundaries, affecting individuals of all ages and with significant variations in severity and triggers. While the exact cause remains a mystery, the impact of asthma on respiratory function is profound, affecting both the structure and function of the respiratory system. This paper aims to shed light on the relationship between asthma and respiratory function while exploring innovative approaches to manage and treat this condition.
Asthma exerts diverse effects on the respiratory system, ranging from structural alterations to functional impairments. Airway remodeling, characterized by increased smooth muscle mass, mucous gland hypertrophy, and subepithelial fibrosis, contributes to the chronic airflow obstruction observed in asthma (Joseph et al., 2022). Furthermore, inflammation within the airways leads to epithelial damage, edema, and increased mucus production, exacerbating airway narrowing and obstruction during asthma attacks. Moreover, bronchoconstriction, a hallmark feature of asthma, results from the hyperresponsiveness of airway smooth muscle cells to various stimuli, including allergens, pollutants, and respiratory infections. This exaggerated broncho-constrictive response further compromises airflow dynamics, exacerbating respiratory symptoms and impairing lung function. Beyond structural alterations, asthma significantly impacts gas exchange and pulmonary function. Ventilation-perfusion (V/Q) mismatching occurs due to regional airflow limitation and altered distribution of pulmonary blood flow, leading to impaired gas exchange and hypoxemia during exacerbations. Additionally, prolonged air trapping and hyperinflation contribute to increased residual volume and reduced expiratory flow rates, exacerbating respiratory distress and limiting exercise tolerance in individuals with severe asthma.
Despite the challenges posed by asthma, there is a ray of hope for those who suffer from it! Addressing the multifaceted nature of asthma requires a comprehensive approach to management, encompassing both pharmacological and non-pharmacological interventions. Recent advancements in asthma treatment are not just about symptom control, but they also aim to reduce exacerbation frequency and mitigate long-term complications. One promising avenue lies in the development of biological therapies targeting specific inflammatory pathways implicated in asthma pathogenesis. Monoclonal antibodies directed against interleukin-5 (IL-5), interleukin-4 receptor alpha (IL-4Rα), and immunoglobulin E (IgE) have shown efficacy in reducing exacerbation rates and improving lung function in severe eosinophilic asthma (Holgate, 2012). Furthermore, precision medicine approaches utilizing biomarkers such as fractional exhaled nitric oxide (FeNO) and peripheral blood eosinophil count aid in identifying individuals likely to benefit from targeted biologic therapies, enabling personalized treatment strategies tailored to the patient’s inflammatory profile. Nonpharmacologic interventions, such as lung conditioning, airway clearance, and patient education programs are important for optimal asthma management. The lung conditioning, accompanied by activities such as exercise training and relaxation exercises, are associated with asthma management education. All of these promote physical condition, symptom control, and psychosocial well-being in individuals with asthma. With patient health being a first and foremost concern, these options should be heavily considered and applied where possible. Moreover, technological innovations, such as smart inhalers and telemedicine platforms, offer novel approaches to monitoring asthma control, enhancing medication adherence, and facilitating remote consultations between patients and healthcare providers. These digital health solutions empower patients to actively engage in their asthma management while enabling timely intervention and support from healthcare professionals.
In summary, asthma poses significant challenges to respiratory function, manifesting in a variety of ways including structural changes, functional impairment, and systemic manifestations. By clarifying the asthma-respiratory health relationship, we can recognize the importance of a multidisciplinary approach to asthma management. Advances in asthma treatment through continued research and collaboration promise to improve outcomes and improve quality of life for individuals living with this chronic respiratory condition.
References:
Holgate S. T. (2012). Innate and adaptive immune responses in asthma. Nature Medicine, 18(5), 673–683. https://doi.org/10.1038/nm.2731
Joseph, C., & Tatler, A. L. (2022). Pathobiology of Airway Remodeling in Asthma: The Emerging Role of Integrins. Journal of asthma and allergy, 15, 595–610. https://doi.org/10.2147/JAA.S267222
Habib, N., Pasha, M. A., & Tang, D. D. (2022). Current Understanding of Asthma Pathogenesis and Biomarkers. Cells, 11(17), 2764. https://doi.org/10.3390/cells11172764.

Ethans project describes in great detail the symptoms, treatments, and the science behind asthma. The objective within this topic is outlined clearly throughout this explanation of asthma. Ethan states that there are about 300 million people who struggle with asthma worldwide. He goes into detail on how asthma affects your lungs and can cause an attack due to the restriction of air within your lungs. Some of the symptoms Ethan described within this project displays shortness of breath, wheezing, coughing, and tightness within the chest. Ethan goes on to explain that there are no ages for people who are prone to asthma. People and children of all ages are prone to asthma, and there is no ideology as to where it comes from, or the cure for it.
Essentially asthma is inflammation within your lungs due to unknown reasons, and the airways become restricted. This results in difficulty breathing along with other symptoms as stated prior. It is stated within project that the increased smooth muscle mass is associated with airway remolding, which produces excess mucus; thus, causing an obstruction within the lungs. Asthma is also associated with affecting the gas exchange within the lungs and having a pulmonary disturbance as well. When air is trapped for prolonged periods of time it leads to hyperinflation, which will lead to respiratory distress. Furthermore, there are many treatments out there to help diminish the symptoms that people may experience with asthma. Most treatments aim to help open up the airway, to help people breath a little easier.
Ethans project goes on to demonstrate clearly a normal lung, versus a lung with asthma. It is clearly visualized that the lung with asthma, has increased tissue and inflammation around the airway. This is where it become difficult to breath.