Neutropenia is a white blood cell (WBC) condition caused by a low number of neutrophils. This is a disease that can have many potential causes including cancer, cancer treatments, bone marrow disorders, many types of infections, immune system disorders, nutrition problems, and chronic idiopathic neutropenia. For this project cancer and cancer treatments that cause neutropenia will be the focus. This will be covering the course objective ‘Relate how the lymphatic system can indicate disease’.
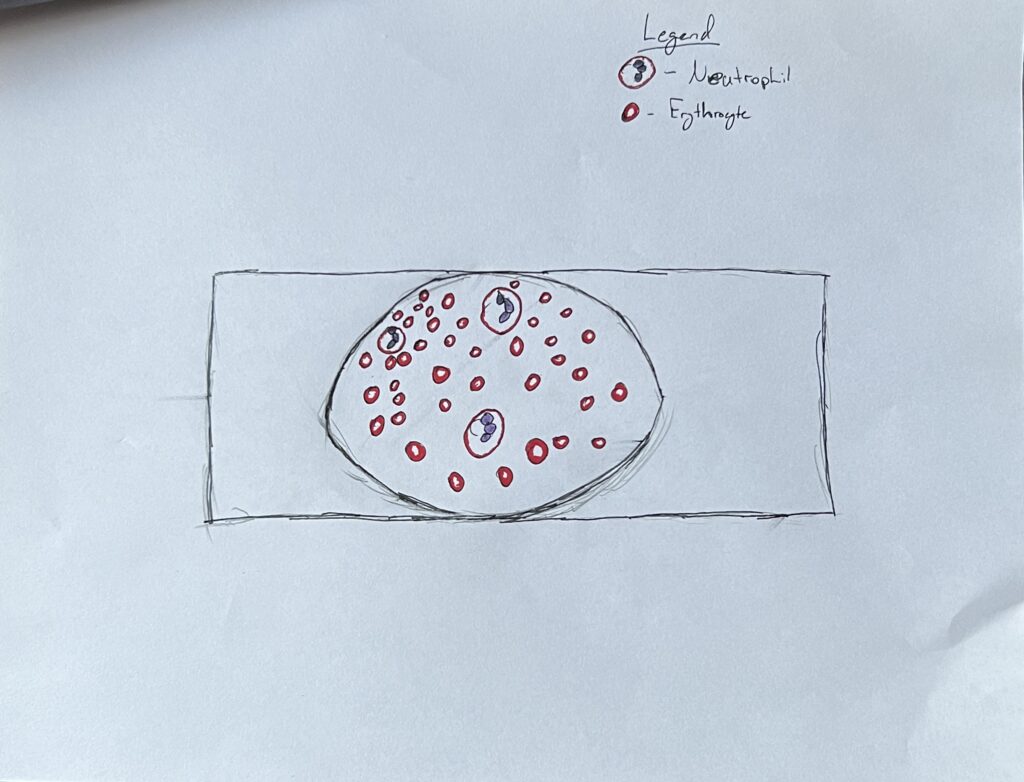
Neutropenia is defined as a decrease in absolute neutrophil count (ANC) to below normal levels (Boxer & Dale, 2022). In layman terms neutropenia is a deficiency in neutrophils, a type of white blood cell. Neutrophils are a granulocyte and type of phagocyte used as part of the body’s defense against infection. Neutrophils work by traveling to the site of infection and ingesting microorganisms before releasing enzymes that destroy them. They also boost the immune response of other immune cells (National Cancer Institute, n.d.). Due to their role in the immune system working to prevent infection, a decrease in the cells has apparent consequences. Often individuals may be unaware that they have neutropenia but as a result of neutropenia secondary conditions may develop, therefore neutropenia may present as: frequent fevers or infections, this can include bladder infections, lung infections, mouth sores, sinus infections, or skin infections (NCCN, 2021). Neutropenia is identified by a diagnostic blood test, a medical team will assess WBC counts and determine if an individual’s ANC is below the designated range for neutropenia, this typically is between 1000-1500 neutrophils/microliter (The American Cancer Society, 2024).
Neutropenia has multiple causes including, cancer and certain cancer treatments. Neutropenia typically occurs when neutrophils in the blood are used up or destroyed faster than they can be produced or when the bone marrow does not produce enough neutrophils. Certain cancers can cause neutropenia such as leukemias, lymphomas, or multiple myeloma (The American Cancer Society, 2024). These conditions all affect the bone marrow and can cause a low ANC by disrupting the production of neutrophils. Cancer treatments can also induce neutropenia in an individual. These can include chemo, certain targeted drug therapies, and bone marrow or stem cell transplants. There are two mechanisms by which drugs can cause neutropenia, immune mediated destruction of circulating neutrophils by drug-dependent or drug-induced antibodies, and direct toxic effects on marrow granulocytic precursors (Coates, 2022). The effects of drug induced neutropenia is the same as that caused by cancer, such as increased susceptibility to infection and fever.
The treatment for neutropenia is dependent on the cause of the neutropenia, but there are a couple common treatments before and after it is identified. If the neutropenia is diagnosed and the patient is febrile, they may be given anti-biotics, anti-virials, anti-fungal, or growth factors to try and prevent infection and produce more white blood cells. For a patient undergoing cancer treatment and chemotherapy their cancer treatment team may work closely with them to manage their condition with medication prophylactically.
Citations
The American Cancer Society . (2024, February 6). Low White Blood Cell Counts: Neutropenia. Low White Blood Cell Counts | Neutropenia | American Cancer Society. https://www.cancer.org/cancer/managing-cancer/side-effects/low-blood-counts/neutropenia.html
Boxer , L., & Dale, D. (2002, April). Neutropenia: Causes and consequences. Seminars in Hematology. https://www.sciencedirect.com/science/article/abs/pii/S0037196302500160
Coates , T. (2022, September 21). Drug-induced neutropenia and agranulocytosis. https://medilib.ir/uptodate/show/8374
National Cancer Institute. (n.d.). NCI Dictionary of Cancer terms. https://www.cancer.gov/publications/dictionaries/cancer-terms/def/neutrophil
NCCN. (2021, March 23). Anemia and Neutropenia . nccn.org. https://www.nccn.org/patients/guidelines/content/PDF/anemia-patient-guideline.pdf
Wingard, J. (2022, May 4). Overview of neutropenic fever syndromes. https://medilib.ir/uptodate/show/16708

Zach’s STEAM project discusses neutropenia, a condition characterized by a low number of neutrophils, a type of white blood cell crucial for fighting infections. Neutropenia can be caused by many things like cancer and cancer treatments, which affect the bone marrow’s ability to produce enough neutrophils. Common symptoms of neutropenia include frequent fevers or infections. Diagnosis of neutropenia requires a blood test t to measure the absolute neutrophil count (ANC). Treatment depends on the underlying cause and can include medications like antibiotics, antivirals, antifungals, or growth factors to stimulate white blood cell production.
Neutropenia’s causes include cancer, cancer treatments, bone marrow disorders, infections, immune system disorders, nutrition problems, and chronic idiopathic neutropenia. Cancer and certain cancer treatments disrupt neutrophil production, leading to a low ANC. Cancer types like leukemias, lymphomas, and multiple myeloma affect bone marrow and can cause neutropenia. Cancer treatments like chemotherapy, targeted drug therapies, and bone marrow or stem cell transplants can also induce neutropenia. Drugs can cause neutropenia by immune-mediated destruction of circulating neutrophils or direct toxic effects on marrow granulocytic precursors. For this reason, treatment depends on the source of neutropenia’s arousal, even more so because there are so many different causes.
Management of neutropenia. Like what was mentioned previously, involves treating underlying causes. If neutropenia is diagnosed, febrile patients may receive antibiotics, antivirals, antifungals, or growth factors to prevent infection and boost white blood cell production. Cancer patients undergoing chemotherapy may receive medication prophylactically to manage neutropenia. Proper management is crucial to prevent infections and complications associated with neutropenia.