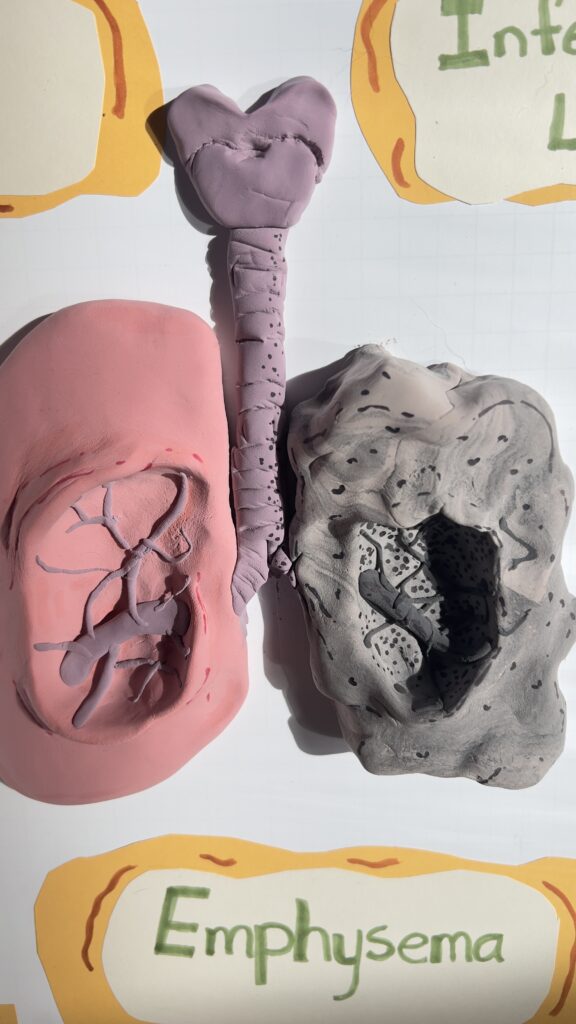
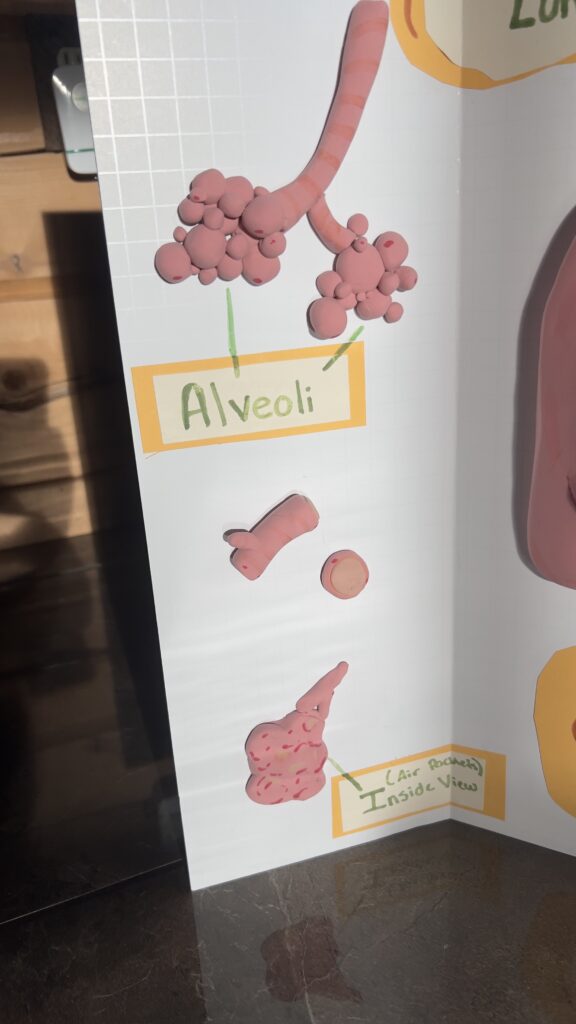
For my STEAM project I’ll be addressing the objective #46 analyzing the effects of disease on the function and structure of the respiratory system for emphysema. For this I’ll explain the origin, effects, how it disturbs the general function and regulation of our respiratory system. Emphysema, is a debilitating lung condition, intricately disrupts the delicate balance of the respiratory system imposing significant challenges to lung health and function. Defined by the irreversible enlargement of airways deep within the lungs, including respiratory bronchioles and alveolar sacs. Emphysema is characterized by the destructive breakdown of these vital structures, devoid of fibrotic tissue regeneration (National Center for Biotechnology Information, n.d.). This pathological alteration severely impairs the exchange of gasses within the lungs, manifesting as obstructive ventilatory defects discernible through spirometry testing.
The origin of emphysema primarily lies in cigarette smoking, a habit that triggers oxidative stress and perpetually undermines lung physiology and tissue equilibrium (Frontiers in Medicine, 2021). Among the labyrinth of lung cells alveolar type II (ATII) cells stand central, bearing the potential to repair injured epithelium. However, in emphysema dysfunctionality pervades these crucial cells, hindering their regenerative capacity. The complexities of emphysema’s progression mechanisms have thus far the discovery of effective treatments, hampered by an incomplete understanding of lung pathophysiology.
Smoking-induced emphysema often culminates in chronic respiratory failure, punctuated by acute exacerbations posing life-threatening risks (National Center for Biotechnology Information, n.d.). Chronic obstructive pulmonary disease (COPD), encompassing emphysema, predicates a relentless decline in lung function and persistent respiratory symptoms like cough and sputum production (European Respiratory Journal, 2004). Nearly half of smokers develop chronic bronchitis, characterized by chronic cough and sputum production without significant airway obstruction.
Understanding the effects of emphysema on respiratory muscle function unveils the profound impact of pulmonary hyperinflation. Alterations in chest wall geometry chronically reduce the apposition zone of the diaphragm, impeding critical inspiratory actions (European Respiratory Journal, 2003). Shortened diaphragm sarcomeres, induced by hyperinflation, further diminish mechanical efficiency, exacerbating respiratory muscle dysfunction. Also oxidative stress and malnutrition, common in COPD patients, contribute to respiratory muscle injury, exacerbating functional impairments.
Despite these adversities, adaptive changes occur within respiratory muscles, particularly the diaphragm, to withstand increased mechanical loads. However, studies indicate a decrease in diaphragm fiber size, not necessarily indicative of typical atrophy, but rather an adaptive response to enhance oxygen transport (European Respiratory Journal, 2003). COPD patients exhibit decreased endurance of inspiratory muscles, exacerbating dyspnea and ventilatory failure during exacerbations.
Inspiratory muscle training emerges as a promising intervention, augmenting muscle strength and endurance. Structural changes observed following training, including an increase in type I fiber proportion and fiber size, suggest a training effect rather than mere injury (European Respiratory Journal, 2003). Comprehensive evaluation and tailored interventions are imperative to address the multifaceted respiratory muscle dysfunction in COPD effectively.
In the end though, emphysema poses significant challenges to respiratory function. From its origins in cigarette smoking-induced oxidative stress to its intricate effects on respiratory muscles, emphysema exacts a toll on lung health. Yet, among these challenges interventions like inspiratory muscle training offer hope for mitigating respiratory muscle dysfunction and improving patient outcomes. Continued research into the complexities of emphysema and its impact on respiratory function is crucial for advancing therapeutic strategies and enhancing the quality of life for affected individuals.
Works Cited
Effects of Smoking on Lung Function: European Respiratory Journal. (2004). Effects of smoking on lung function: The importance of smoking cessation in COPD patients. https://erj.ersjournals.com/content/erj/23/3/464.full.pdf
Emphysema and the Respiratory System: National Center for Biotechnology Information. (n.d.). Emphysema and the respiratory system.
https://www.ncbi.nlm.nih.gov/books/NBK539910
Pathophysiology of Emphysema: Frontiers in Medicine. (2021). Pathophysiology of emphysema: A systematic review.
https://www.frontiersin.org/articles/10.3389/fmed.2021.762878/full
Respiratory Muscle Dysfunction in COPD: European Respiratory Journal. (2003). Respiratory muscle dysfunction in COPD: A comprehensive analysis.
https://erj.ersjournals.com/content/erj/22/46_suppl/41s.full.pdf

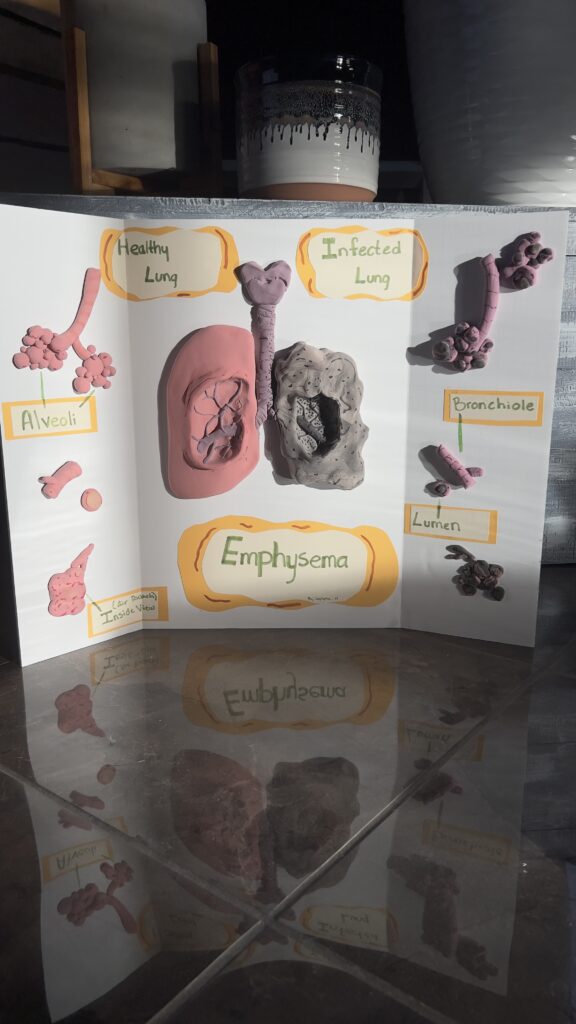
Jaylynn’s STEAM project focuses on the lung condition, Emphysema, and its effects on the structure and function of the respiratory system; and she portrayed this through clay art. Emphysema is a condition that develops in the lungs by exposure to pollutants, specifically cigarette smoking. This exposure leads to irreversible enlargement of the bronchioles and alveolar sacs. Emphysema can also lead to other respiratory conditions such as bronchitis, chronic obstructive pulmonary disease, chronic cough, and more. As for treatment, inspiratory muscle training has been shown to be an effective treatment for its ability to develop muscle strength and endurance for patients suffering from emphysema.