Our liver is one of the largest organs in our body. The liver plays a central role in all metabolic processes in the body. Blood flows from the digestive organs through the portal vein to the liver carrying nutrients, waste, and toxic substances. Once they reach the liver, they are processed, stored, detoxified, and passed back into the blood or released into the intestines to be eliminated. Klatskin tumors can affect the functions of the liver and when it has metastasized, surrounding organs and lymph nodes.
3% of all gastrointestinal tumors originating from either the intra- or extrahepatic bile duct epithelium are considered cholangiocarcinomas, making them rare. (Sharma & Yadav, 2018) Cholangiocarcinomas that originate from the hepatic Patients can present with symptoms which can include jaundice, abdominal pain and weight loss, fatigue, nausea, dark urine and clay-colored stools. (Soares, Kamel, Cosgrove, Herman, & Pawlik, 2014) Although most patients have very few symptoms and only come to the attention of medical professionals because of jaundice or abnormalities in routine bloodwork. (Jarnagin & Winston, 2005)
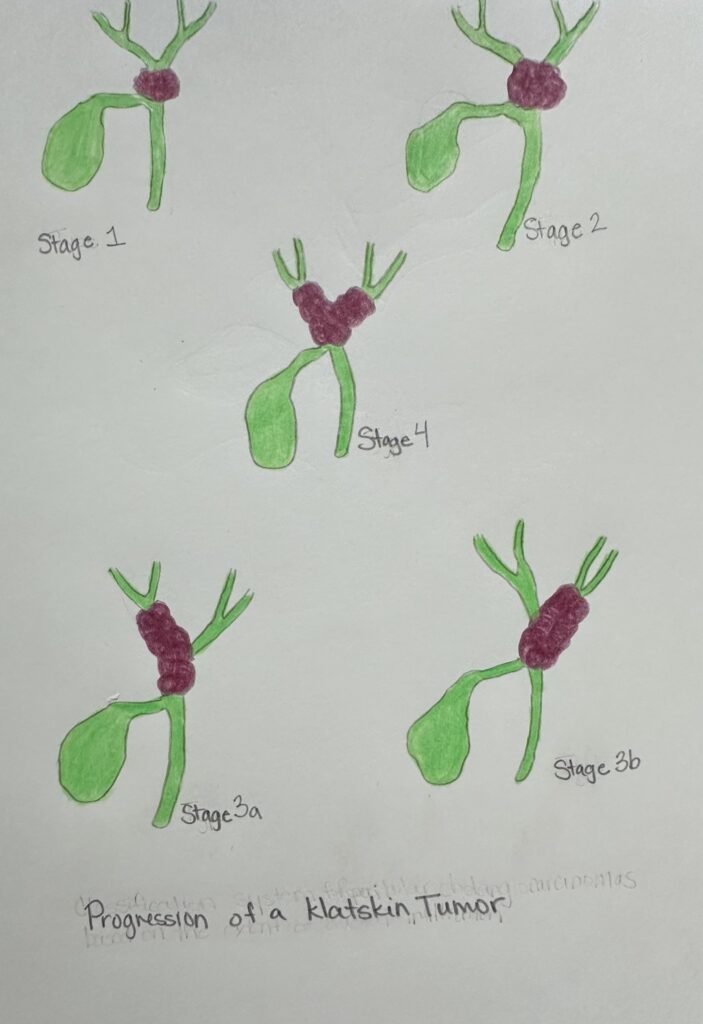
Staging of Klatskin tumors is done with computed topography (CT), magnetic resonance imaging (MRI) and ultrasound to define the stage of the tumor. There are five stages to this disease. Stage I is where the tumor is distal to the hepatic duct junction, Stage II is where the tumor extends and involves the hepatic duct junction, Stage IIIA is where the tumor involves the hepatic duct junction and the proximal right hepatic duct, Stage IIIB is where the tumor involves the hepatic duct junction and the proximal left hepatic duct, and Stage IV is where the tumor extends into the bilateral proximal hepatic ducts and up to the seminal bile ducts. (Soares, Kamel, Cosgrove, Herman, & Pawlik, 2014) Metastasis to surrounding lymph nodes and the peritoneum is common in Klatskin tumors due to the thin bile duct wall.
Ascites can develop in the advanced stages of the disease when the tumor has metastasized to the peritoneum causing the ascitic fluid to leak and build up in the abdomen. Ascites can also develop due to portal hypertension as there is increased pressure within the portal venous system due to the tumor affecting the hepatic ducts. (Kalra, Yetiskul, Wehrle, & al, 2023) When the tumor metastasizes to the surrounding lymph nodes, it can then be spread throughout the body via the lymphatic system, causing tumors to arise in distant organs. The lymphatic drainage pathway of the hilar bile duct follows one of three paths: from the hepatic artery to the celiac lymph nodes, along the bile duct to the para-aortic lymph node, or along the portal vein to the superior mesenteric node. (Li, Zhou, Ma, Li, & Deng, 2020) Blockage of the hepatic ducts can also hinder digestion as bile that is produced in the liver cannot make its way to the intestines. This in turn causes jaundice as there are increased bilirubin levels in your blood.
Once a person is diagnosed with a Klatskin tumor, depending on the stage, the 5-year survival rates are as follows: 87% for Stage I, 61% for Stage II, 45% for Stage IIIA, 30% for Stage IIIB, and 11% for Stage IV. The only treatment associated with long term survival is surgical resection. (Ebata, et al., 2017) Most often 20-30% of patients diagnosed with a Klatskin tumor are at a stage where surgical resection is an option. Most Klatskin tumors are deemed unresectable due to the metastatic spread to other organs, the peritoneum and lymph nodes. The first line of treatment for advanced stages of Klatskin tumors is a combination of chemotherapy with immune checkpoint inhibitors. (Saud Dar, et al., 2024) Within 12 months of diagnosis, a majority of patients with unresectable tumors often die from hepatic failure or complications secondary to biliary obstruction.
References
Ebata, T., Ercolani, G., Alvaro, D., Ribero, D., DiTommaso, L., & Valle, J. W. (2017). Current Status on Cholangiocarcinoma and Gallbladder Cancer., 6, pp. 59-65. doi:10.1159/000449493
Jarnagin, W., & Winston, C. (2005). Hilar cholangiocarcinoma: diagnosis and staging. HPB, 7, 244-251. doi:10.1080/13651820500372533
Kalra, A., Yetiskul, E., Wehrle, C., & al, e. (2023, May 1). Physiology, Liver. Retrieved from National Library of Medicine: https://www.ncbi.nlm.nih.gov/books/NBK535438/
Li, J., Zhou, M.-H., Ma, W.-J., Li, F.-Y., & Deng, Y.-L. (2020). Extended lymphadenectomy in hilar cholangiocarcinoma: What it will bring? World Journal of Gastroenterology, 26(24), 3318-3325. doi:10.3748/wjg.v26.i24.3318
Saud Dar, F., Abbas, Z., Ahmed, I., Atique, M., Aujla, U. I., Azeemuddin, . . . al, e. (2024). National guidelines for the diagnosis and treatment of hilar cholangiocarcinoma. World Journal of Gastroenterology, 30(9), 1018-1042. doi:10.3748/wjg.v30.i9.1019
Sharma, P., & Yadav, S. (2018). Demographis, tumor characteristics, treatment, and survival of patients with Klatskin tumors. Annals of Gastroenterology, 31, 213-236. doi:10.20524/aog.2018.0233
Soares, K. C., Kamel, I., Cosgrove, D. P., Herman, J. M., & Pawlik, T. M. (2014). Hilar cholangiocarcinoma: diganosis, treatment options, and management. Hepatobiliary Surgery and Nutrition, 3(1), 18-34. doi:10.3978/j.issn.2304-3881.2014.02.05

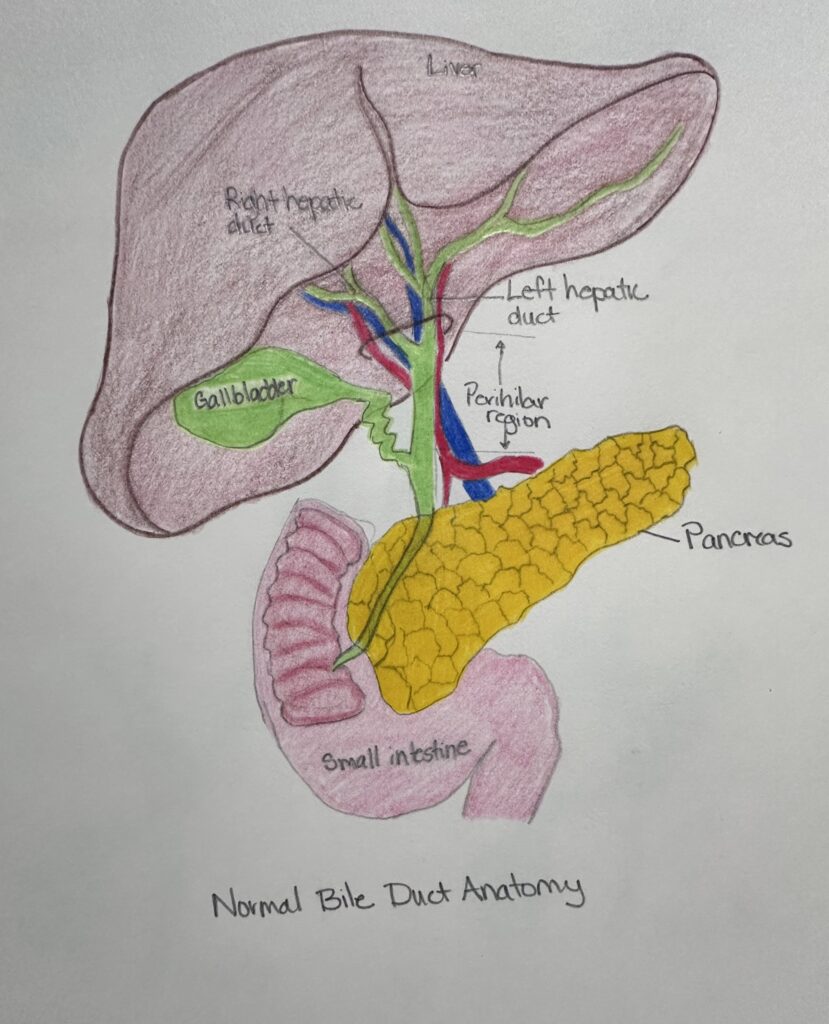
Elizabeth Kirchgessner’s project is about the effects of a Klatskin tumor on the liver. I believe her objective is “relate how the lymphatic system can cause disease”, because she describes how a Klatskin tumor can affect the lymphatic system.She uses two drawing presentations to help explain her research. The first drawing is a visual representation of the anatomy of the liver and bile duct anatomy. This image includes the small intestine, pancreas and gallbladder. The second drawing shows the progression of a Klatskin tumor from stages one to four, she displays the tumor in green and the hepatic duct in purple. Beth explains to us that the liver is essential for all metabolic processes that happen within the body including the transportation of nutrients and waste. The liver is the site of storage, detoxification and circulation. After she gives background information on liver processes, she informs us that the Klatskin Tumor greatly impacts liver function. She then goes on to talk about tumors of the gastrointestinal area and the associated symptoms which include: weight loss, fatigue, dark urine, or clay colored stool. Beth explains that most patients present with no symptoms at all. She describes the stages of the Klatskin tumor starting with Stage one, where the tumor is at the distal to the hepatic junction. Stage 4 is the most advanced, where we will find extension of the tumor bilateral of the hepatic junction. This stage is displayed in the middle of her second image. You can see the visual of the tumor and its bilateral progression. Beth ties her research into her objective when she describes ascites and how the lymphatic system pathways are contributors to the spread of the Klatskin tumor and additionally, when she explains how the hepatic artery blockage is responsible for the liver dysfunction. Beth closes with treatment outcomes if one is diagnosed with a Klatskin tumor on the liver, which vary from a promising prognosis from Stage 1 to a poor prognosis for Stage 4.
Elizabeth Kirchgessner’s project is about the effects of a Klatskin tumor on the liver. I believe her objective is “relate how the lymphatic system can cause disease”, because she describes how a Klatskin tumor can affect the lymphatic system.She uses two drawing presentations to help explain her research. The first drawing is a visual representation of the anatomy of the liver and bile duct anatomy. This image includes the small intestine, pancreas and gallbladder. The second drawing shows the progression of a Klatskin tumor from stages one to four, she displays the tumor in green and the hepatic duct in purple. Beth explains to us that the liver is essential for all metabolic processes that happen within the body including the transportation of nutrients and waste. The liver is the site of storage, detoxification and circulation. After she gives background information on liver processes, she informs us that the Klatskin Tumor greatly impacts liver function. She then goes on to talk about tumors of the gastrointestinal area and the associated symptoms which include: weight loss, fatigue, dark urine, or clay colored stool. Beth explains that most patients present with no symptoms at all. She describes the stages of the Klatskin tumor starting with Stage one, where the tumor is at the distal to the hepatic junction. Stage 4 is the most advanced, where we will find extension of the tumor bilateral of the hepatic junction. This stage is displayed in the middle of her second image. You can see the visual of the tumor and its bilateral progression. Beth ties her research into her objective when she describes ascites and how the lymphatic system pathways are contributors to the spread of the Klatskin tumor and additionally, when she explains how the hepatic artery blockage is responsible for the liver dysfunction. Beth closes with treatment outcomes if one is diagnosed with a Klatskin tumor on the liver, which vary from a promising prognosis from Stage 1 to a poor prognosis for Stage 4.