Course objectives: {1, 2, 3, 53}
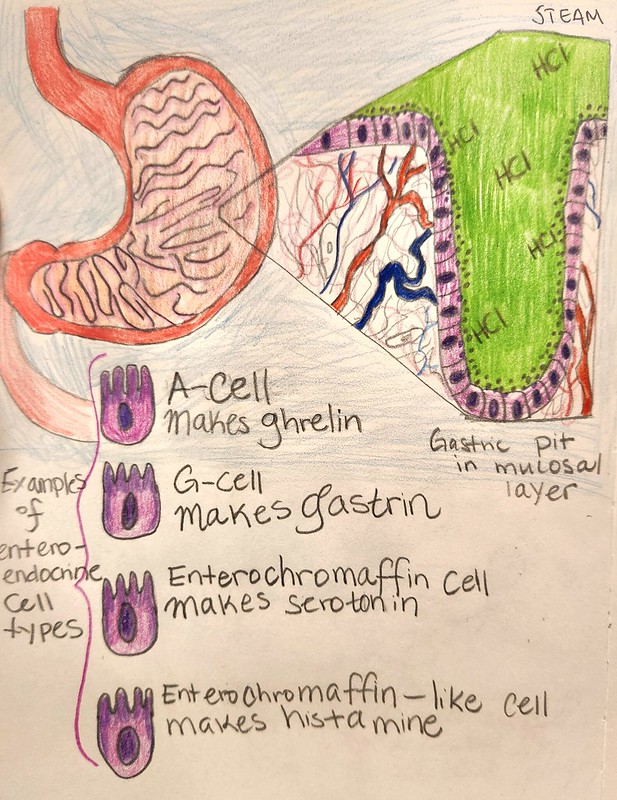
The gastrointestinal tract has recently been recognized for its impact beyond digestion and into the realm of endocrine function. While the majority of the gut is made up of enterocytes which line the lumen and protect the rest of the organ, it contains pits or crypts that contain cells capable of producing hormones, called enteroendocrine cells. The gut produces dozens of hormones and can be considered the largest endocrine organ in some respects (Gunawardene et al., 2011). Enteroendocrine cells are important components of the gastric pits and intestinal crypts throughout the alimentary canal.
The mucosal lining of the stomach can secrete serotonin, histamine, and GABA (Dockray et al., 1996). Serotonin has numerous effects in the central nervous system and is important for promoting “bowel motility, bladder control, and cardiovascular function” (Sheffler & Pillarisetty, 2019). Serotonin in the central nervous system is involved in learning, memory, mood, stress responses, addiction, sex drive, fear, anger, appetite, and a bevy of other functions (Berger et al., 2009). Histamine helps with motivation-based behavior, including eating patterns. It also can keep one more alert and awake. GABA is one of the premier inhibitory neurotransmitters. It can also secrete ghrelin, gastrin, and somatostatin. (Ricardo-Silgado et al., 2021). Ghrelin is a hormone that influences the organism to take in food, increases the emptying of the stomach into the duodenum, and decreases the amount of insulin that gets secreted. Insulin and ghrelin are antagonistic to each other, with one suppressing the other’s secretion (Ricardo-Silgado et al., 2021). Leptin is also antagonistic to ghrelin and it is made by white adipose tissue. Leptin signals satiety among other functions. (Dornbush & Aeddula, 2020) Somatostatin is an inhibitory hormone to growth hormone. It also represses the secretion of several other hormones including thyroid hormone and in the gastrointestinal tract: secretin and gastrin (“Somatostatin”, n.d.). Gastrin is produced in part in the stomach and encourages the body to produce gastric acid and enzymes for digestion of intake. This is also another function of histamine.
Enteroendocrine hormone concentrations have been implicated to contribute to many conditions including depression, irritable bowel disease, and obesity. There is ongoing research as to their effects on the immune system as well such as having toll-like receptors for sensing pathogens as part of the innate immune system (Moran et al., 2008). Interestingly, bacteria present farther down in the gut such as the colon can influence the secretion of enteroendocrine hormones including galanin which is important for the hypothalamic-pituitary-adrenal axis and many survival mechanisms and behaviors–e.g. sensing pain and eating (Appleton 2018). Some bacterial metabolites, short-chain fatty acids, can modulate the amount of serotonin released by the enterochromaffin cells, one of more than a dozen enteroendocrine cell types. More than 95% of the serotonin in the body is manufactured by the epithelial cells of the gut (Appleton 2018). As previously described, serotonin is implicated in processes relating to mood and behavior, so it makes sense that impaired functioning of the enteroendocrine cells is under investigation for connections to mood disorders such as depression.
The study of the endocrine role of the gut is a rapidly expanding field in science and connections between the gut and other parts of the body, especially the brain, are crucial to our understanding of physiology. The stomach can produce several of these chemicals, many of which feedback to the digestive system itself, but others of which affect distant systems through the bloodstream. To recap, the stomach’s secreted hormones include serotonin, histamine, GABA, ghrelin, somatostatin, and gastrin.
Bibliography
Appleton J. (2018). The Gut-Brain Axis: Influence of Microbiota on Mood and Mental Health.
Integrative medicine (Encinitas, Calif.), 17(4), 28–32. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6469458/#:~:text=The%20gut%2Dbrain%20axis%20is,routes%20of%20communication%20as%20well.
Berger, M., Gray, J. A., & Roth, B. L. (2009). The expanded biology of serotonin. Annual review
of medicine, 60, 355–366. https://doi.org/10.1146/annurev.med.60.042307.110802
Dockray, G. J., Varro, A., & Dimaline, R. (1996). Gastric endocrine cells: gene expression,
processing, and targeting of active products. Physiological reviews, 76(3), 767–798.
https://doi.org/10.1152/physrev.1996.76.3.767
Dornbush, S., & Aeddula, N. R. (2020). Physiology, Leptin. PubMed; StatPearls Publishing.
https://www.ncbi.nlm.nih.gov/books/NBK537038/
Gunawardene, A. R., Corfe, B. M., & Staton, C. A. (2011). Classification and functions of
enteroendocrine cells of the lower gastrointestinal tract. International journal of
experimental pathology, 92(4), 219–231.
Moran, G. W., Leslie, F. C., Levison, S. E., Worthington, J., & McLaughlin, J. T. (2008).
Enteroendocrine cells: neglected players in gastrointestinal disorders?. Therapeutic
advances in gastroenterology, 1(1), 51–60. https://doi.org/10.1177/1756283X08093943
https://doi.org/10.1111/j.1365-2613.2011.00767.x
Ricardo-Silgado, M. L., McRae, A., & Acosta, A. (2021). Role of Enteroendocrine Hormones in
Appetite and Glycemia. Obesity medicine, 23, 100332.
https://doi.org/10.1016/j.obmed.2021.100332
Sheffler, Z. M., & Leela Sharath Pillarisetty. (2019). Physiology, Neurotransmitters.
Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK539894/
Somatostatin: What It Is, Function & Symptoms. (n.d.). Cleveland Clinic.
https://my.clevelandclinic.org/health/articles/22856-somatostatin