(SARS)-CoV-2, or COVID-19, took the world by storm in March of 2020 when the World Health Organization (WHO) declared COVID-19 a pandemic. On December 11, 2020 the Food and Drug Administration (FDA) gave emergency use authorization (EUA) to a vaccine developed by Pfizer-BioNTech for those 16 or older. A week later Moderna was given an EUA for their vaccine for those 18 or older. There was a lot of hesitancy for people to get the vaccine because of how quickly the vaccine was developed, but this isn’t entirely true. mRNA vaccines, as used in the COVID-19 vaccine, have been thoroughly researched since the early 2000s.
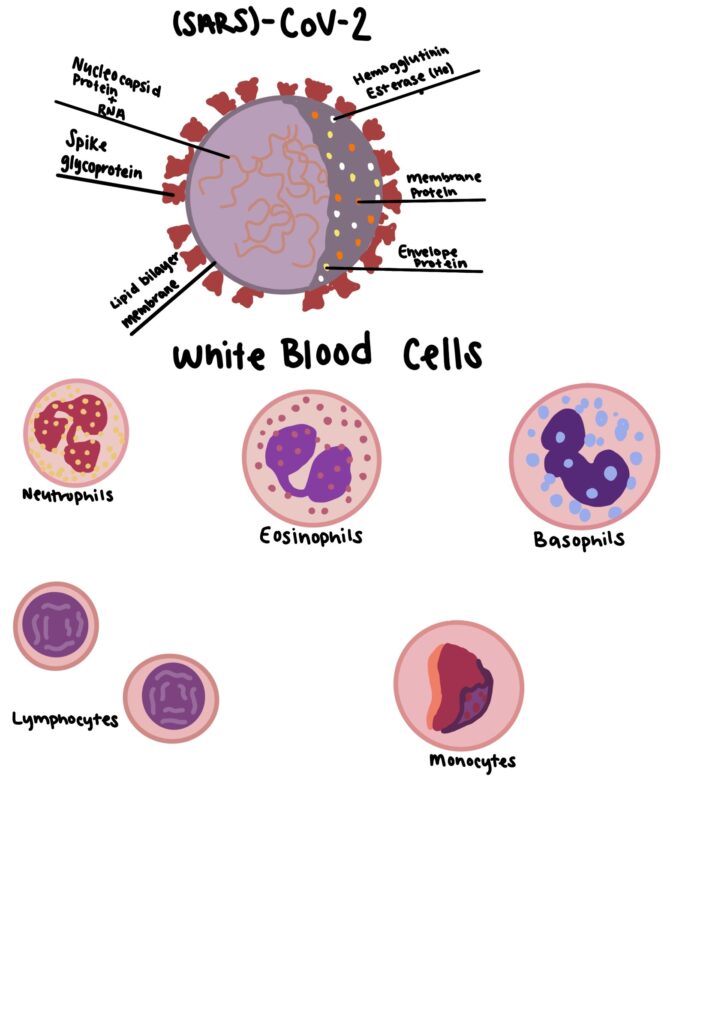
Changes in white blood cell (WBC) counts can reflect the immune response that we see in individuals with COVID-19. A retrospective study performed in Tongji Hospital in Wuhan, Hubei province, China looked at the WBC counts of survivors and non-survivors of the COVID-19 virus. Wuhan is often regarded as the epicenter of the COVID-19 pandemic as it was when the first known cases of (SARS)-CoV-2 were reported. “Levels of eosinophils, lymphocytes and basophils in non-survivors were significantly lower than those in survivors. Death rate in low eosinophils group was higher and no patient died in normal eosinophils group. Moreover, positive correlation was found between the counts of lymphocytes and eosinophils in patients with glucocorticoids use but not in patients without the treatment.” (Tong, Xunliang et al. “Characteristics of peripheral white blood cells in COVID-19 patients revealed by a retrospective cohort study”). Lymphocytes play a crucial role in maintaining immune homeostasis during viral infections. (SARS)-CoV-2 has been shown to activate both innate and adaptive immune responses, so changes of peripheral blood cells can indicate immune damage caused by the viral infection.
The hygiene hypothesis is a theory that exposure to certain benign microorganisms can help protect our bodies against allergies by strengthening our immune systems, meaning that exposure will strengthen our immune system and allow for a lesser reaction when infected with more serious diseases. Some scientists have theorized that the hygiene hypothesis can also explain the susceptibility to the COVID-19 virus. “Trained immunity can be induced raises the prospect of its exploitation to raise the threshold of resistance to COVID-19 infection, a valuable maneuver during the time when we have yet to develop effective treatments or vaccines” (Sehrawat and Rouse “Does the Hygiene Hypothesis Apply to Covid-19 Susceptibility”). Although there are now multiple vaccines with FDA approval, at the time of this article there were none. Having a strengthened innate immune system can be vital to dampening the symptoms of viruses through “frequent exposure of individuals to natural environmental microbes, live attenuated vaccines against other viruses or bacteria or certain natural ligands such as different types of lectins and saponins that can stimulate innate immune receptors all help to reduce the clinical consequences of COVID-19 infection” (Sehrawat and Rouse).
The hygiene hypothesis and WBC counts can be combined for future therapies in atopic disease and disorders of immune dysregulation and continued development for other diseases as well. “Research over the past 10 years provides evidence connecting the commensal and symbiotic microbes (intestinal microbiota) and parasitic helminths with immune development, expanding the hygiene hypothesis into the “microflora” and “old friends” hypotheses, respectively. There is evidence that parasitic helminths and commensal microbial organisms co-evolved with the human immune system and that these organisms are vital in promoting normal immune development.” Knowing that the hygiene hypothesis typically stands true, barring other factors like autoimmune diseases that suppress the immune system, and that WBC counts can indicate what type of immune response will occur through retrospective studies, further development can occur in vaccine creation.
Works Cited
Sehrawat, Sharvan, and Barry T. Rouse. “Does the Hygiene Hypothesis Apply to Covid-19 Susceptibility?” Microbes and Infection, Oct. 2020, www.ncbi.nlm.nih.gov/pmc/articles/PMC7347347/.
Stiemsma, Leah T., et al. “The Hygiene Hypothesis: Current Perspectives and Future Therapies.” ImmunoTargets and Therapy, 27 July 2015, www.ncbi.nlm.nih.gov/pmc/articles/PMC4918254/.
Tong, Xunliang, et al. “Characteristics of Peripheral White Blood Cells in COVID-19 Patients Revealed by a Retrospective Cohort Study.” BMC Infectious Diseases, 9 Dec. 2021, bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-021-06899-7#Abs1.

Anna did her STEAM project on how Covid-19 and the hygiene hypothesis interact. When SARS-COV-2 became a pandemic in 2020, people were wary of the vaccines because of how fast they were developed. However, mRNA vaccines have been researched since the 2000s. A study in Wuhan, China found that levels of eosinophils, lymphocytes, and basophils were significantly lower in non-survivors, than those who survived the covid infection. SARS-COV-2 has shown that it can activate both the innate and adaptive immune responses. This can indicate changes of peripheral blood cells which show immune damage caused by SARS-COV-2. The hygiene hypothesis theory states that exposure to benign microorganisms can help protect against diseases and strengthen our immune system. “Trained immunity” may raise the threshold of resistance to COVID-19 infection. This can mean having a strengthened innate immune system may lead to lesser symptoms of viruses through the frequent exposure of microbes. Parasitic helminths can be considered vital to developing normal immune function.