Unit nine showed the reproductive system and the development and inheritance of childbirth. One of the main objectives was to explain common disorders during pregnancy and their cause. In this essay and with the images provided, I will be covering preeclampsia which has the potential to be a dangerous pregnancy complication. This paper includes causes, symptoms, effects, and possible treatments for preeclampsia.
Preeclampsia is a pregnancy-specific hypertensive disorder that can affect almost every organ system and complicates 2-8% of pregnancies globally (Lee, 2022). Prenatal screening and early detection are critical for effective treatments and management of preeclampsia. However, preeclampsia screening is solely based on maternal risk factors and has low detection rates.
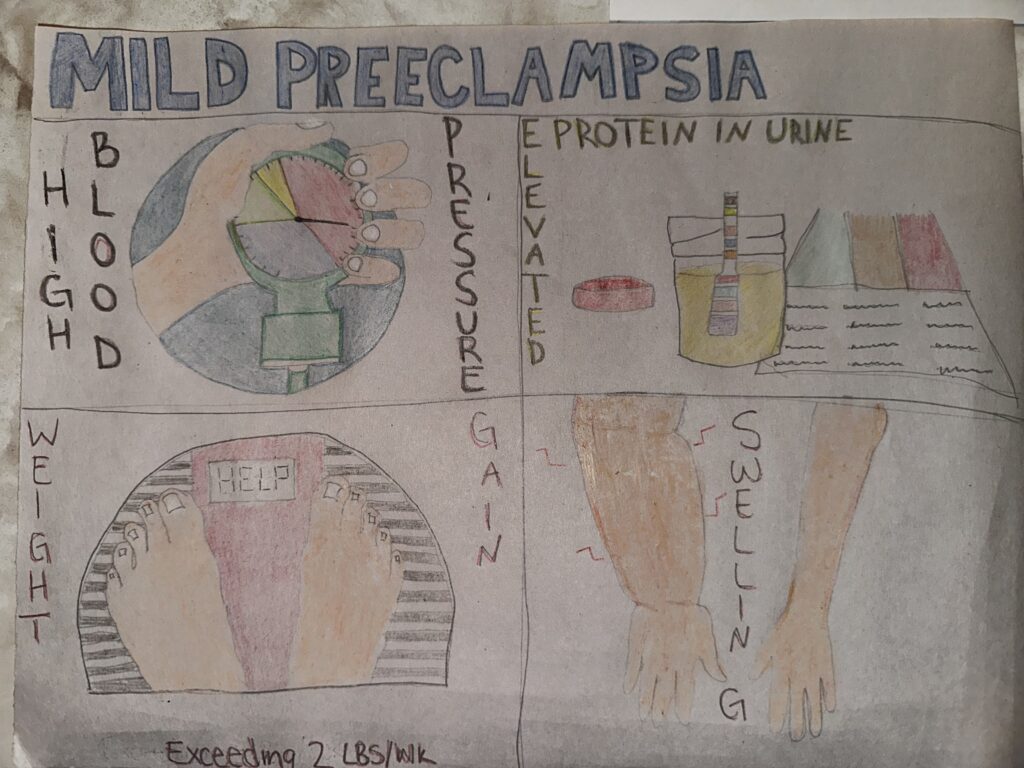
A way you can detect preeclampsia is through the symptoms that manifest. One of the symptoms is high blood pressure or high levels of protein in your urine. This could also indicate trouble with your kidneys or liver (Preeclampsia Foundation, n.d.). How to detect high levels of protein is to see if urine is foamy, frothy, or bubbly, urinating more often, and experiencing muscle cramps at night.
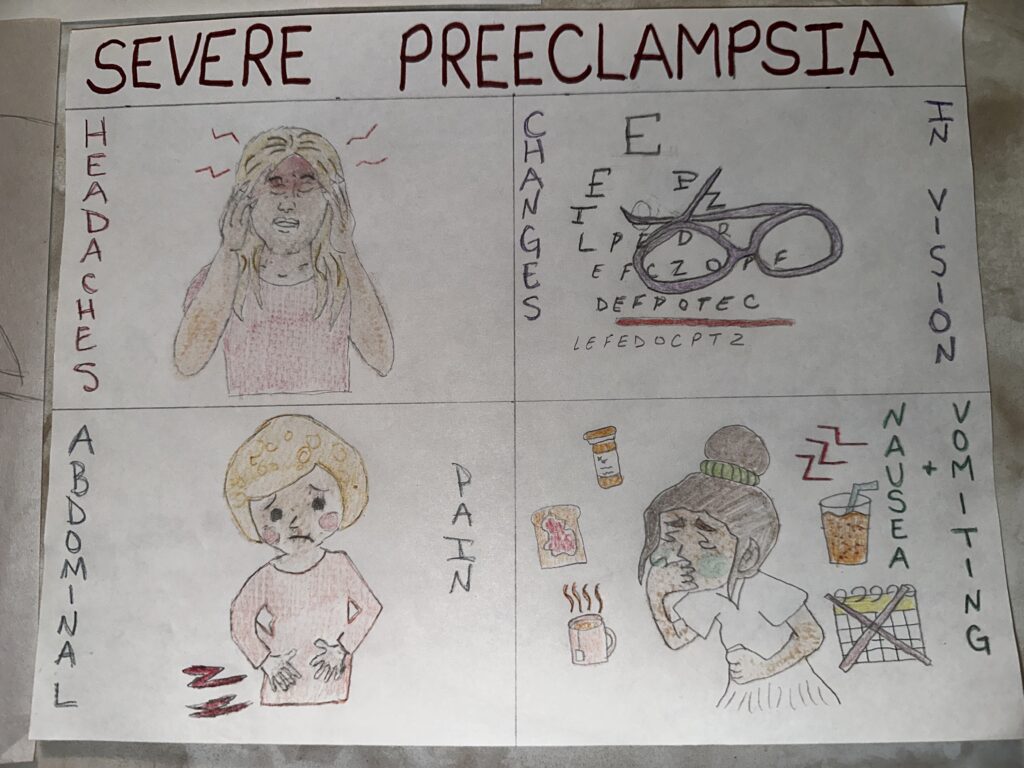
Other symptoms of preeclampsia are decreased blood platelets, which cause easy or excessive bruising, superficial bleeding into the skin that appears as a rash of pinpoint-sized reddish-purple spots, prolonged bleeding from cuts, and blood in urine or stool. Lastly, the more alarming symptom is signs of brain trouble or fluid in the lungs (Preeclampsia Foundation, n.d.). Some indications of these symptoms are seizures and/or visual disturbances, coughing up blood or bloody froth, and difficulty breathing while lying down. Some of these symptoms also indicate more common, less frightening diseases, so it is suggested to consult a doctor.
Preeclampsia was once called, “the disease of theories,” but research efforts this past decade have produced some breakthroughs in improving diagnosis and prediction, and led to prevention and treatments (Preeclampsia Foundation, n.d.). There are some leading theories when it comes to the causes of preeclampsia. Some of these theories include poor or not enough blood flow to the uterus, inflammation, disruption of the balance of hormones that maintain the diameter of the blood vessel, calcium deficiency, injury to the blood vessels due to excessive blood flow or pressure, nutritional deficiencies, obesity, and genetic tendency (Preeclampsia Foundation, n.d.).
After diagnosis of any disease, one may ask, “Well, what do I do now?” The treatment decisions for preeclampsia depend on how severe the condition is, the potential for maternal complications, how far along the pregnancy is, and the potential risks to the fetus. If the pregnancy is at 37 weeks or later, the healthcare provider will want to deliver the fetus to treat preeclampsia and avoid further complications. If the pregnancy is at less than 37 weeks and depending on the health of the woman, a healthcare provider may consider options that give the fetus more time to develop (USDHHS, n.d.).
With preeclampsia, there are long-term effects after you give birth known as postpartum preeclampsia. Patients in the postpartum period remain at risk for the development of hypertension disorders in the postpartum period and long-term sequelae related to a prior diagnosis of preeclampsia. These patients also carry an increased risk of major morbidity and mortality throughout their lives beyond the immediate postpartum period (Bisson, 2023).
Overall, while preeclampsia is a common pregnancy disorder, if not caught early or treated properly, it could lead to further complications such as eclampsia, organ damage, or even maternal and fetal mortality. Fortunately, there are various methods and tests available for early diagnosis of preeclampsia, including regular blood pressure monitoring, urine protein testing, and other prenatal screenings. By promptly identifying and managing preeclampsia, healthcare providers can recommend a healthy course of action, which may involve lifestyle modifications, medication, or close monitoring, thereby minimizing the risk of long-term effects on the woman carrying the fetus and ensuring a safer pregnancy outcome for both mother and baby.
References
Bisson, C. M., Dautel, S. E., Patel, E., Suresh, S. C., Dauer, P., & Rana, S. (2023). Preeclampsia pathophysiology and adverse outcomes during pregnancy and postpartum. Frontiers in Medicine, 10. https://doi.org/10.3389/fmed.2023.1144170
Lee, K., Brayboy, L. M., & Tripathi, A. (2022). Preeclampsia: A scoping review of risk factors and suggestions for future research direction. Regenerative Engineering and Translational Medicine, 8(3), 394–406. https://doi.org/10.1007/s40883-021-00243-w.
Preeclampsia Foundation. (n.d.). Cause of preeclampsia. https://www.preeclampsia.org/cause-of-preeclampsia.
Preeclampsia Foundation. (n.d.). Signs and symptoms of preeclampsia. https://www.preeclampsia.org/signs-and-symptoms.
U.S. Department of Health and Human Services. (n.d.). What are the treatments for preeclampsia, eclampsia, & HELLP syndrome? Eunice Kennedy Shriver National Institute of Child Health and Human Development. https://www.nichd.nih.gov/health/topics/preeclampsia/conditioninfo/treatment.

Rania’s objective was to describe a potentially fatal condition that can occur during pregnancy, spotlighting unit 9 talking about the reproductive system and fetal development. She starts off by talking about what preeclampsia is itself – high blood pressure that is caused by pregnancy. The most common symptom is a high blood pressure reading that can be caught in the early stages while the condition is still mild. Other mild symptoms include weight gain, protein in urine, and swelling. Thanks to 21st-century medicine, we can more easily and quickly detect preeclampsia and take steps to mitigate it. If not caught in time or not treated, it can ultimately lead to death, even after pregnancy. Post-pregnancy preeclampsia can lead to several complications in the long run, including being at risk of the development of hypertension disorders and having an increased risk of major morbidity and mortality for the rest of their lives. There are many theories around what exactly causes preeclampsia, but so far known risk factors include obesity, blood flow to the uterus, inflammation, disruption of the balance of hormones that maintain the diameter of the blood vessel, and calcium deficiency.