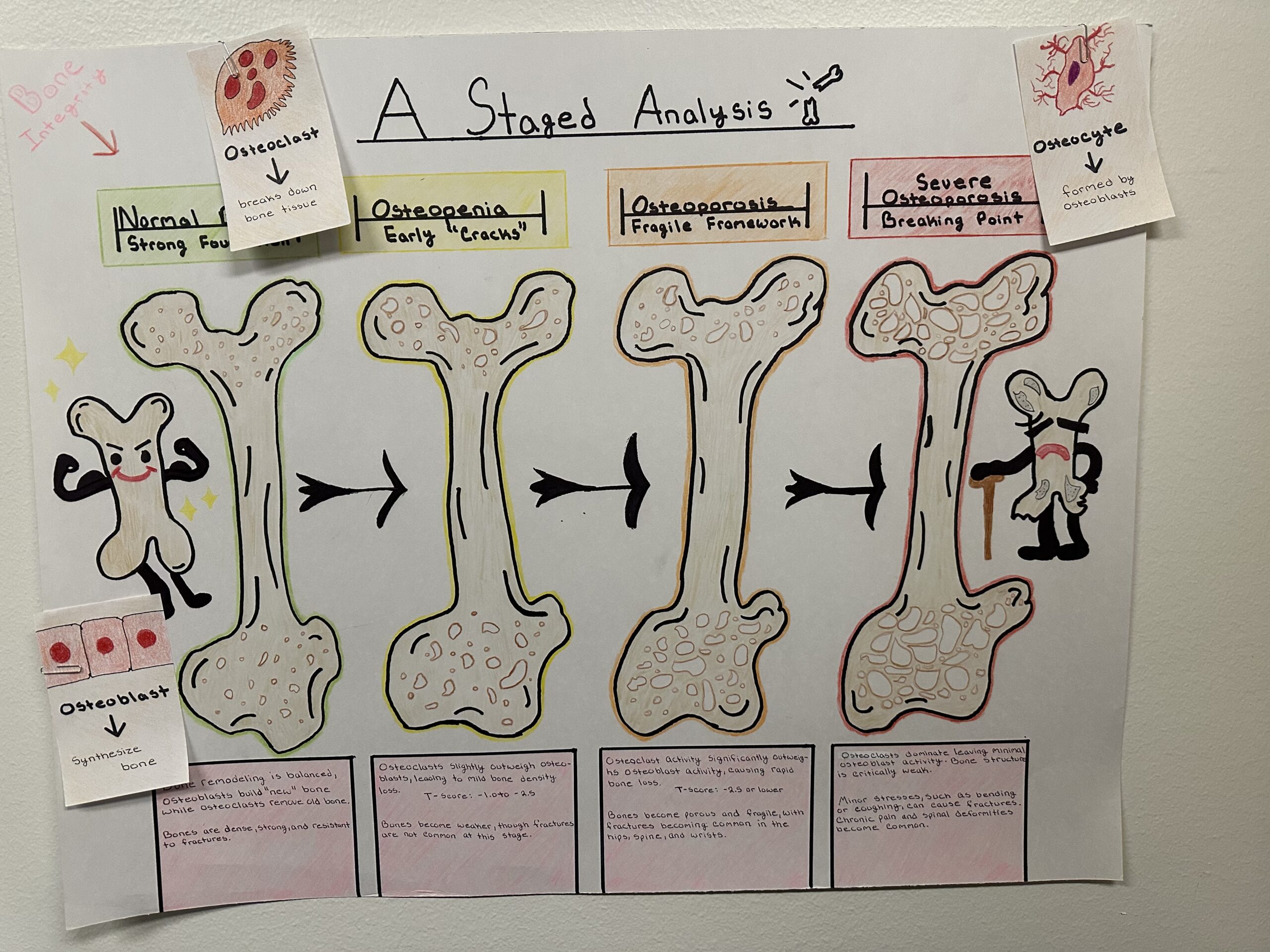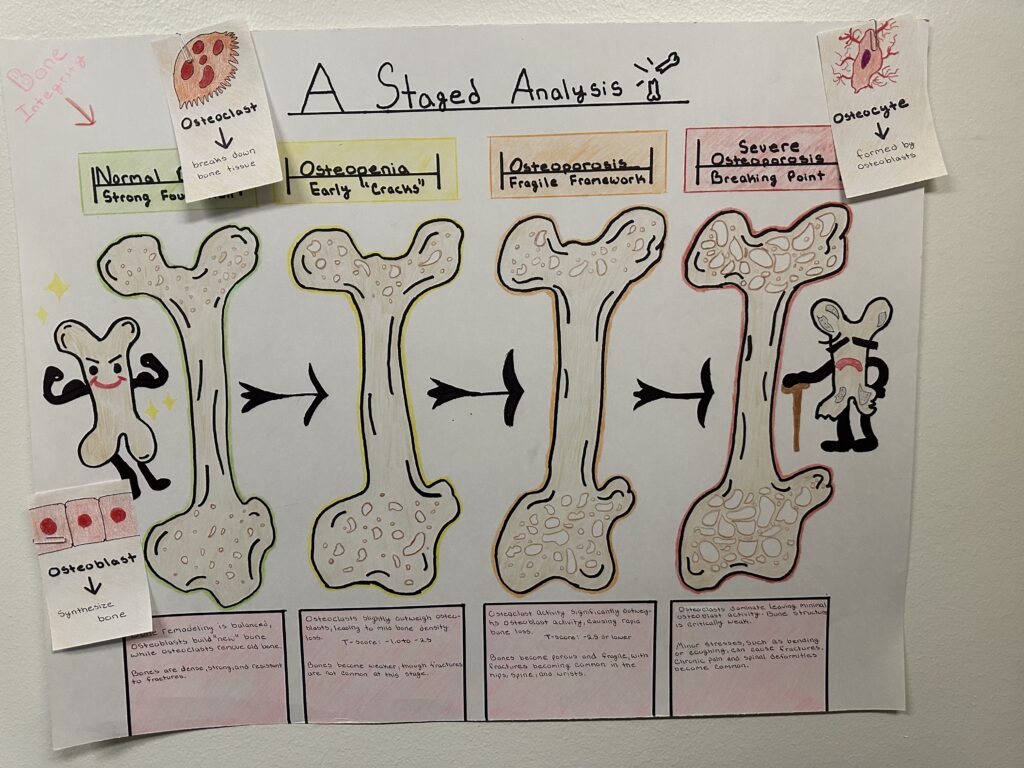
Bones provide structure, protection, and mobility for the body. However, as we age, the balance between bone formation and breakdown shifts, leading to conditions like osteoporosis (the silent disease). This condition weakens bones over time, increasing the risk of fractures. My poster board, illustrates how osteoporosis progresses through four stages, showing the changes in bone structure and density over time. These stages, along with the role of hormones and preventive measures, offer a basic understanding of how the disease develops and how it can be managed.
The first “stage” is healthy bone, bones are dense and balanced, this is due to bone remodeling. This continuous cycle replaces old or damaged bone tissue with new tissue, two main bone cell tissues are involved. Osteoblasts, which build/synthezise bone, and osteoclasts, which break it down. When these two processes remain balanced, the structure of trabecular (spongy) and cortical (outer) bone layers remains intact, as shown in the first section of the poster. Early signs are classified as osteopenia. At this stage, trabecular bone starts to thin, which can lead early bone loss. While bones remain strong, their ability to withstand stress decreases. Without intervention, this leads to osteoporosis, the third stage. Here, bone density significantly declines, and the microarchitecture of the bone deteriorates. Also, increased risk of fractures in areas like the hips, wrists, and spine. In the fourth stage, severe osteoporosis, bones become so fragile that even minor movements, such as bending or coughing, can cause fractures. Spinal deformities like kyphosis, depicted in your poster as a hunched back, often result from repeated compression fractures in this stage.
The progression of osteoporosis is influenced by hormonal changes, aging, and lifestyle choices. Hormones are critical regulators of bone remodeling. Estrogen, for example, suppresses osteoclast activity, preventing excessive bone breakdown. However, during menopause, estrogen levels drop, which accelerates bone loss. Other hormones, such as parathyroid hormone (PTH), calcitonin, and vitamin D, also play roles. PTH increases osteoclast activity when calcium levels are low, while calcitonin reduces it, acting as a counterbalance. Vitamin D (calcitriol), supports calcium absorption from the diet, ensuring sufficient minerals for bone formation. Chronic deficiencies in any of these hormones can disrupt the bone remodeling process, accelerating the stages of osteoporosis (Clarke & Khosla, 2015).
Lifestyle choices also factors into osteoporosis. Smoking and excessive alcohol intake reduce osteoblast activity, while physical inactivity decreases mechanical stress on bones, limiting the stimulation needed to maintain density. Diet intake, especially in calcium, vitamin D, and magnesium, further weaken bones.
Preventive measures and treatments like regular exercise, particularly weight-bearing and resistance activities, strengthens bones by promoting osteoblast activity. A diet rich in calcium, vitamin D, and vitamin K2 supports bone health by ensuring proper mineralization and directing calcium to bones rather than soft tissues. Regular bone density screenings, such as dual-energy X-ray absorptiometry (DEXA), can detect early bone loss and allow for timely interventions (Ji et al., 2021). Medications like bisphosphonates, denosumab, and modern therapies like romosozumab target specific pathways in the bone remodeling cycle. These treatments either slow bone resorption or stimulate bone formation, reducing fracture risk in advanced stages of the disease.