In recent years, with the accelerated pace of social life, work pressure, and the prevalence of bad habits, the proportion of people with high blood pressure has gradually increased, and the incidence of cardiovascular diseases in society has also gradually climbed, which myocardial infarction has become the focus of people’s concern. Cardiovascular disease (CVD) and breast cancer (BC) are significant causes of mortality globally, imposing a substantial health burden. The common risk factors for cardiovascular disease, such as hypertension, diabetes, obesity, aging, and physical inactivity, are discussed, emphasizing their modifiability. (Obeidat, O., Charles, K. R., Akhter, N., & Tong, A. 2023)
This topic will focus on the pre-symptoms, causes, and effective prevention methods of cardiovascular diseases, especially myocardial infarction, to draw attention and vigilance to heart health.
Reasons for the increase of cardiovascular diseases in society
The fast-paced life of modern society, high-pressure work, intense competition, poor dietary habits, and lack of exercise have created favorable conditions for the increase of cardiovascular diseases. Studies have shown that poor lifestyles, such as excessive stress, diets high in fats and sugar, and long-term lack of exercise, are directly and closely related to the occurrence of cardiovascular diseases. Today, there is also a gradual increase in the number of people with high blood pressure, which is usually a silent disease; as a result, people with high blood pressure may fail to recognize the severity of their condition and thus fail to follow a treatment plan. The result is usually a heart attack or stroke. Hypertension may also lead to aneurysms (swelling of blood vessels due to weak vessel walls), peripheral arterial disease (blockage of blood vessels in the body’s peripheral regions), chronic kidney disease, or heart failure.
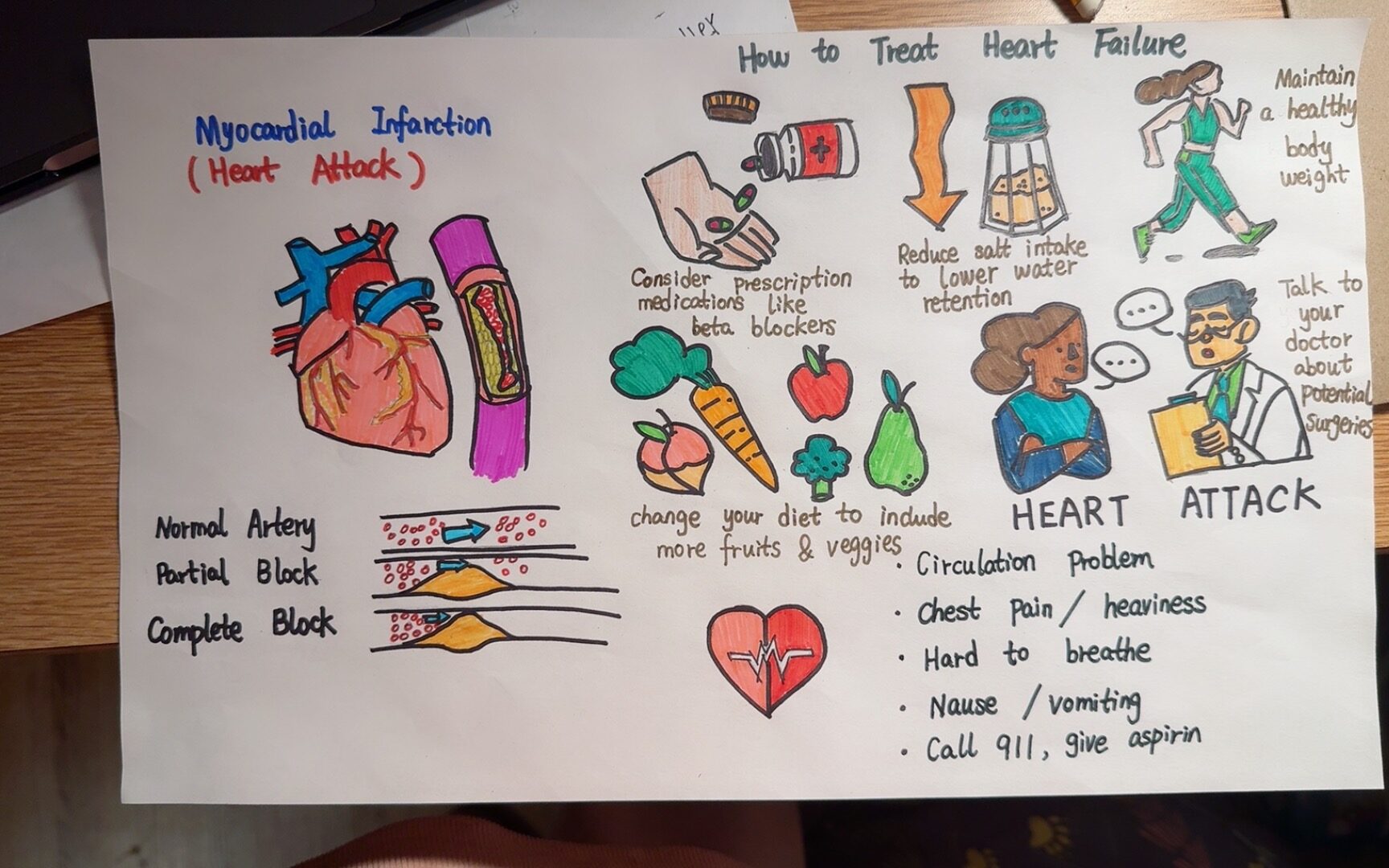
Pre-symptoms of myocardial infarction
Pre-myocardial infarction symptoms are often the “yellow light” of the disease, reminding us to pay attention to heart health. Common symptoms include:
- Chest pain or discomfort: The patient may feel heaviness or pressure in the chest or experience severe chest pain.
- Shortness of breath: Difficulty breathing and shortness of breath are typical symptoms of myocardial infarction.
- Pain or discomfort in arms or shoulders
- Feeling weak, lightheaded, or faint
- Pain or discomfort in the jaw, neck, or back
- Cold sweats and nausea: Patients may experience cold sweats, nausea, and vomiting, accompanied by dizziness and lightheadedness at times.
- Stomach or abdominal discomfort.
- Irregular heartbeat: palpations
(Birnbach, B., Höpner, J., & Mikolajczyk, R. 2020).
Know the path of blood through the heart and circulatory system(Unit11 Cardiovascular and Circulatory Systems Objectives):
Blood enters the right atrium from the somatic circulation through the superior vena cava and inferior vena cava, then is pushed into the right ventricle, enters the pulmonary circulation through the pulmonary artery, becomes oxygenated blood after gas exchange through the pulmonary capillaries, returns to the left atrium, then is pushed into the left ventricle, and finally enters the somatic circulation through the aorta, which transports the oxygenated blood to all tissues and organs of the body. The heart plays a vital role in maintaining normal body functions. (Lecture note: Cardiovascular and Circulatory Systems P25 see attached picture)
Causes of Heart Attack
Myocardial infarction (MI) is the official term for what is commonly referred to as a heart attack. Myocardial infarction is usually caused by a lack of blood flow and oxygen to the region of the heart, resulting in the death of heart muscle cells. Myocardial infarction usually occurs when a buildup of atherosclerotic plaque consisting of lipids, cholesterol, fatty acids, and white blood cells blocks the coronary arteries. Myocardial infarction also occurs when a portion of unstable atherosclerotic plaque crosses the coronary artery system and blocks one of the smaller vessels. The resulting blockage restricts blood and oxygen flow to the heart muscle, resulting in the death of heart muscle tissue. (Anatomy and Physiology 2e 19.1 Heart Anatomy)
What is the connection between heart disease, such as heart attack, and blood circulation pathways?
Heart disease is usually caused by impeded circulation or an inadequate blood supply. As mentioned above, blood circulates through the heart, which acts as the body’s pumping mechanism to transport blood throughout the body while delivering oxygen to all parts.
In heart attacks and other heart diseases, insufficient blood supply to the arteries leads to ischemia or necrosis of the heart muscle. This ischemia or necrosis is usually caused by coronary artery disease (e.g., atherosclerosis), which leads to narrowing or blockage of the coronary arteries, preventing the heart from receiving adequate oxygen and nutrients. Therefore, the close relationship between heart disease and blood circulation pathways means that the progression and severity of heart disease is closely related to the smoothness of blood circulation.
Ways to prevent heart disease.
- Take beta-blockers on time: Medications prescribed by your doctor should be taken regularly to help control blood pressure and reduce the burden on your heart.
- Reduce salt intake: Excessive salt intake is closely associated with high blood pressure, and a moderate reduction in salt intake is essential for heart health.
- Maintain good fitness habits to stay in shape: Regular moderate aerobic exercise and weight control can help maintain a healthy cardiovascular system.
- Eat plenty of fruits and vegetables: Fruits and vegetables rich in vitamins, minerals, and fiber can help lower cholesterol levels and maintain a healthy heart.
- Seek medical advice if you have any discomfort: If you experience chest pain, shortness of breath, or other unusual symptoms, it is vital to seek medical advice promptly and undergo a thorough physical examination to ensure early detection and treatment.
By focusing on cardiovascular diseases, raising public awareness of heart health, and taking proactive and effective preventive measures, we can better protect our hearts, reduce the incidence of cardiovascular diseases, and embrace a healthier and more fulfilling life. Let’s work together to make heart health the bottom line of life.
Citation:
Anatomy and Physiology 2e 19.1 Heart Anatomy & 20.4 Homeostatic Regulation of the Vascular System
Birnbach, B., Höpner, J., & Mikolajczyk, R. (2020). Cardiac symptom attribution and knowledge of the symptoms of acute myocardial infarction: a systematic review. BMC Cardiovascular Disorders, 20, 1-12.Explain the structure and function of the heart.
Obeidat, O., Charles, K. R., Akhter, N., & Tong, A. (2023). Social Risk Factors That Increase Cardiovascular and Breast Cancer Risk. Current Cardiology Reports, 25(10), 1269-1280.
Lecture note: Cardiovascular and Circulatory Systems P25