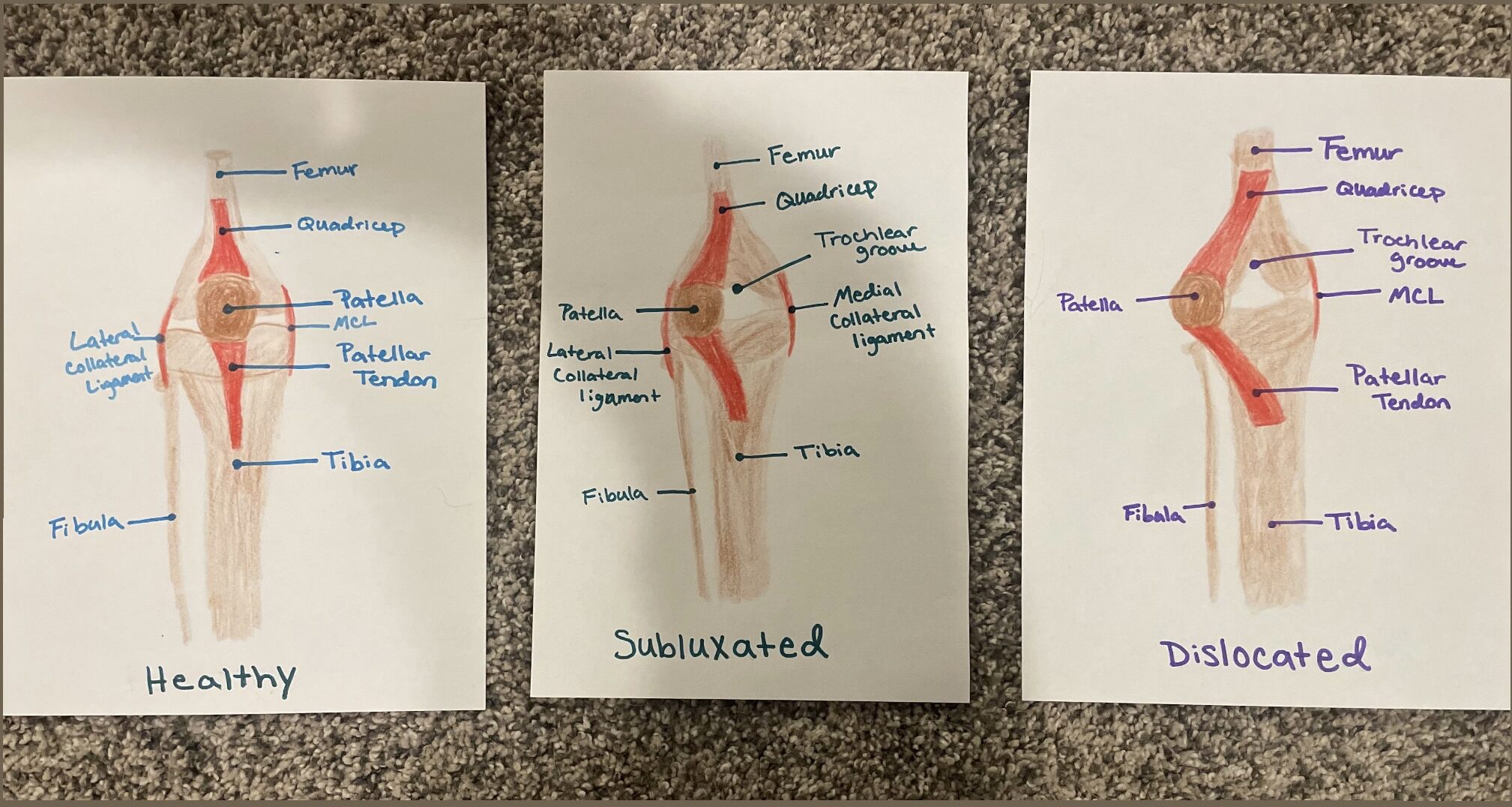
My STEAM project looks at patellar dislocation (PD) in both adolescents and adults as well as covers the objectives “know the structure of the knee joint” and “know the muscles involved in the knee joint.” For the art portion of my project, I chose to draw out a visual image of what a healthy knee, a subluxed knee, and a dislocated knee look like from the posterior view.
The kneecap is found in the front of the femur and is attracted to both the femur and tibia by tendons called patellar tendons. The kneecap plays a vital role in protecting the quadriceps tendons from frictional forces and serves as an attachment spot for the patellar ligament and quadriceps tendon. The structure of the kneecap slightly resembles a wedged shape and sits in a groove in the femur called the trochlear groove (U.S. NLM, 2024). This is where the kneecap can slide and move around when the knee is bent or straightened. There are also two menisci located on the joint surface of the tibia, and one is located laterally while the other is medial. Menisci are made of fibrous cartilage and allow for the kneecap to turn a few degrees inward or outward. Patellar (kneecap) dislocation occurs when the kneecap pops out laterally of the groove it typically sits in, often resulting in the surrounding tendons, such as the meniscus, being stretched and torn, causing damage, inflammation, and pain (Orthopedics & Sports Medicine, 2017). There are different levels of severity when it comes to PD. In some cases, the knee cap can fully move outside of the groove and need assistance to get placed back into the groove. In other cases, which tend to be more mild, the knee cap only partially slides out of its normal place in the groove and is able to pop itself back into place without assistance. Both instances risk damaging the surrounding muscles and tendons and result in symptoms such as rapid swelling, pain, discoloration, and instability (Shneider & Saper, 2021).
Patella dislocation can occur in both adolescents and adults; however, it is most commonly seen in adolescents and young adults around the ages of 14–20 years old (Boston Children’s Hospital, n.d.). PD is also seen more in females and children who participate in sports such as soccer, hockey, gymnastics, or other sports that involve the tibia to rotate outwards at the knee joint. In both adolescents and adults, the more an individual experiences patella dislocations, the more unstable the knee gets due to the stretching of the surrounding ligaments and the more likely they will have further dislocations in the future. Dislocations typically get worse the more they occur, and the risk of damaging ligaments and bones increases significantly after each reoccurrence.
There are different levels of treatments available to help reduce dislocations and permanently prevent them based on how severe the dislocations are and how much damage has occurred to the surrounding ligaments. If subtle subluxation of the knee cap occurs or it is an individual’s first dislocation and no severe damage was done, then the main focus would be to maintain leg, quadriceps, and hip strength by seeing a physical therapist and using a brace to help with swelling and alignment. In more severe cases, when the patella fully slides out of the trochlear groove and damage is done to ligaments such as the meniscus, then surgery is often required. Surgeries focus on realigning the kneecap by reconstructing the medial patellofemoral ligament, making it tight again, and pulling the kneecap back in line with the groove. These surgeries can vary depending on the age of the patient. If the surgery is being done on an adolescent, only tendons and muscles will be reconstructed to realign the patella, whereas in adults, since their bones are fully developed, the bone can be cut to help shift the patella over and create a deeper groove so the kneecap will not be able to slide around as easily and prevent dislocations. With proper treatment and consistent physical therapy, patients can make a full recovery within 2–6 months (Patellar Instability, 2023).
References used:
Sinikumpu, J., & Nicolaou, N. (2023). Current concepts in the treatment of first-time patella dislocation in children and adolescents. Journal of Children’s Orthopaedics, 17(1), 28–33. https://doi.org/10.1177/18632521221149060
U.S. National Library of Medicine. (2024, March 8). In brief: How does the knee work?. InformedHealth.org [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK561512/#:~:text=The%20kneecap%20is%20located%20in,tibia%20by%20the%20patellar%20tendon.
Patellar Dislocation | Orthopedics & Sports Medicine. (2017, August 11). https://health.uconn.edu/orthopedics-sports-medicine/conditions-and-treatments/where-does-it-hurt/knee/patellar-dislocation/#:~:text=Symptoms,apprehension%20that%20problem%20will%20recur.
Patellar instability. (2023, November 1). Johns Hopkins Medicine. https://www.hopkinsmedicine.org/health/conditions-and-diseases/patellar-instability#:~:text=The%20patella%20(kneecap)%20attaches%20to,the%20knee%20bends%20and%20straightens.
Shneider, D. A., & Saper, M. (2021). Medial patellar subluxation without prior surgery: Diagnosis and treatment. Arthroscopy the Journal of Arthroscopic and Related Surgery, 37(1), e25. https://doi.org/10.1016/j.arthro.2020.12.050
