Introduction: STEAM Model Description
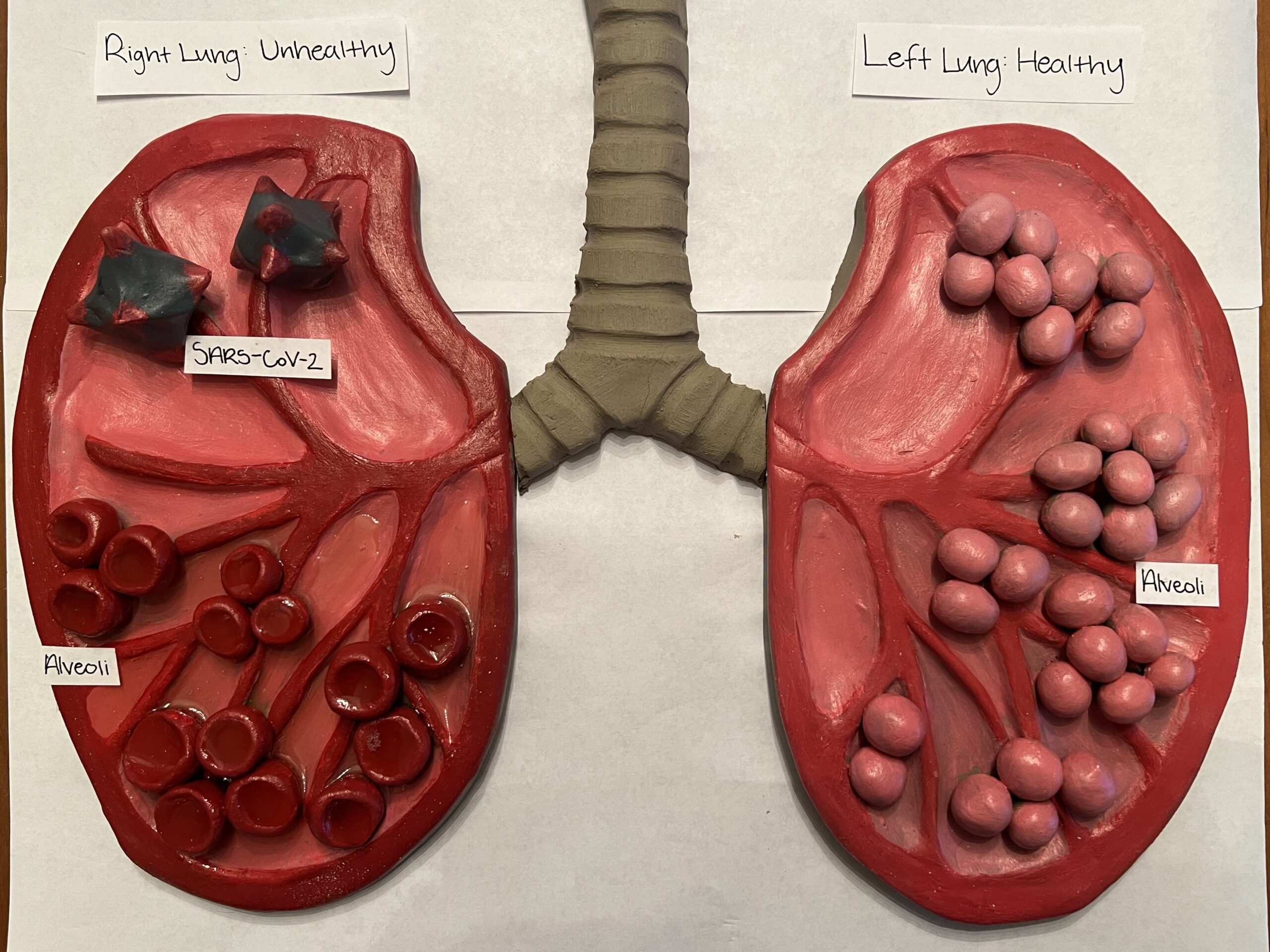
My STEAM project explores the effects COVID-19 pneumonia has on the respiratory system. It explores the infection process, pneumonia development, and how it affects the respiratory system. To develop my project, I utilized clay sculpting to formulate the base, and majority, of my piece. Then, I added smaller details by painting the various parts and applying resin over the sculpture. My project addresses the course objective, “Analyze the effects of disease on the function and structure of the respiratory system.” To showcase this, I displayed the processes and effects COVID-19 pneumonia poses on the lungs in a side-by-side comparison between the infected, left-lung, and the healthy, right-lung.
Part one: COVID-19 Infection
Coronavirus disease 2019, or as commonly referred to as COVID-19, is caused by a member of the coronaviridae family, SARS-CoV-2 (Alipoor et al., 2020). Positive-stranded RNA viruses envelop the structure of coronaviruses (Alipoor et al., 2020). This characterization means that these viruses have positive-sense, single-stranded genomes made of ribonucleic acid that allow the genome to act as messenger RNA and can be directly translated into viral proteins by the host cell’s ribosomes–alluding to the process of infection and replication by SARS-CoV-2. Also assisting infection, viral capsid proteins–such as spike glycoprotein, are vital for cell entry and taking over the healthy cells in infected patients (Alipoor et al., 2020). These numerous methods of infection provide SARS-CoV-2 with effective and relatively easy contraction, as well as replication.
The lung tissue is especially susceptible to infection of SARS-CoV-2 due to the method of airborne contraction and the influence of the Renin-Angiotensin-Aldosterone system (RAAS) in the lungs. COVID-19 is contracted through airborne means, in other words, when someone comes in contact with the droplets and particles of SARS-CoV-s exhaled from an infected individual, contaminated cells become infected (Clevland Clinic., 2022). This often happens when one person inhales these particles into the airways–causing these respiratory cells to be infected. The cells of the respiratory system and the lungs are especially susceptible to SARS-CoV-2 infection due to their involvement in RAAS. There are two different types of RAAS pathways–traditional and non-classic (Mascolo et al., 2021). In the lungs, the traditional RAAS pathway poses detrimental effects on lung tissue and can lead to various pulmonary diseases (Mascolo et al., 2021). To counteract these negative effects, non-classic RAAS exerts a protective effect on the lungs. In doing so, an essential component–the transmembrane angiotensin-converting enzyme-2 (ACE2)–is utilized (Mascolo et al., 2021). However, this specific membrane protein is a susceptible receptor for the viral entry of SARS-CoV-2 (Mascolo et al., 2021). The airborne nature of how COVID-19 is contracted and the susceptibility to infection of respiratory cells make the lungs common targets of SARS-CoV-2 infection.
Part two: COVID-19 Pneumonia
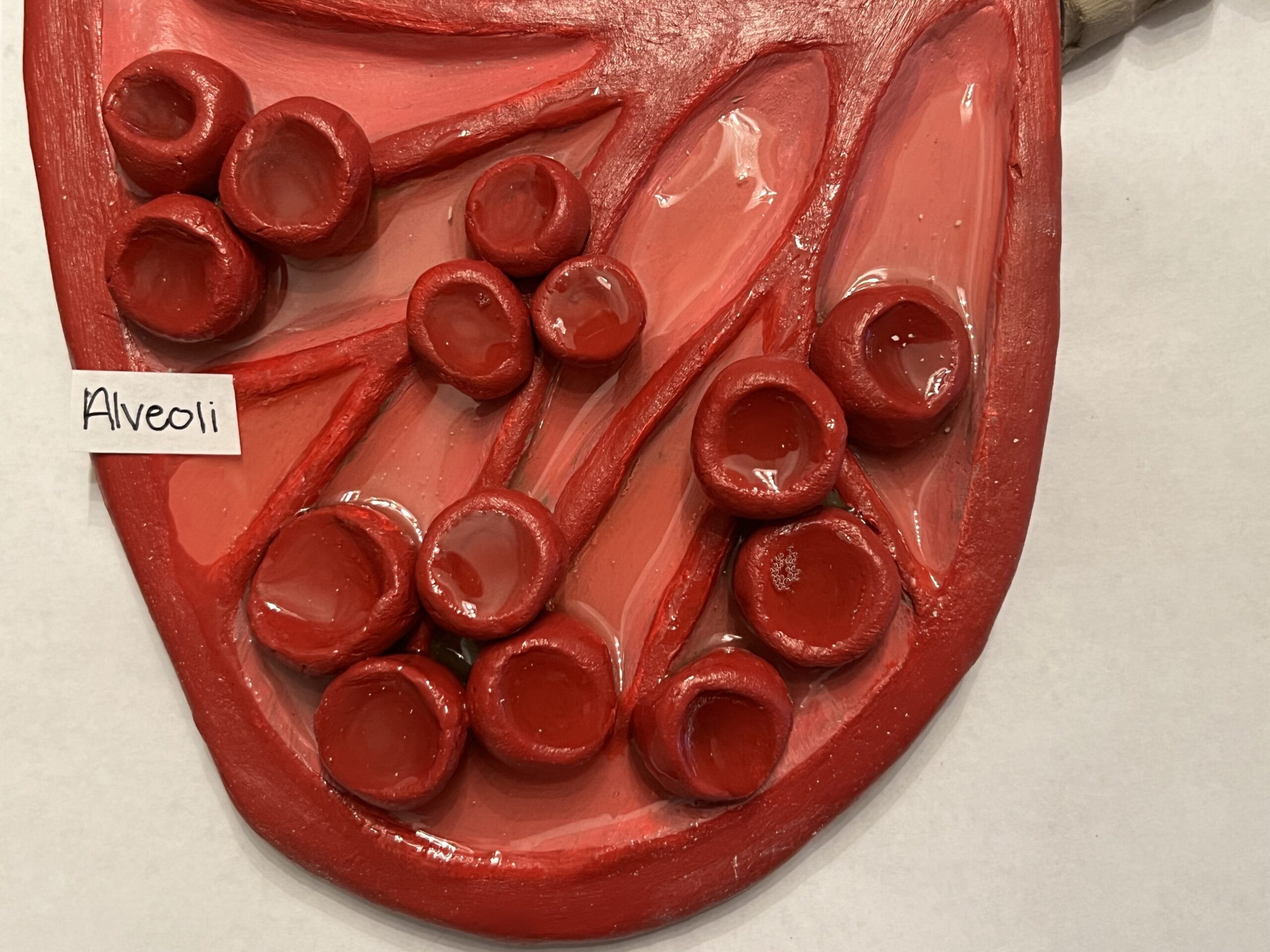
During infection, vital epithelial tissue cells are specifically targeted by SARS-CoV-2, which can lead to pneumonia. Alveolar epithelial type two cells (AEII) are responsible for the defensive mechanisms of the lungs by generating the restrictive alveolar epithelial barrier and also secreting pulmonary surfactant–which reduces surface area tension at the pulmonary air-liquid interface (Yuan et al., 2021). These AEII cells are reportedly more susceptible to SARS-CoV-2 infection (Alipoor et al., 2020)–leading to cell death by pyroptosis and apoptosis (Yuan et al., 2021). Due to AEII cells being the main contributors to pulmonary surfactant production, the decrease in these cells causes increased pressure on the alveoli–eventually leading to their collapse (Alipoor et al., 2020). This system results in the destruction of the epithelium composing alveolar walls.
The inflammatory response–that results in pneumonia–is caused by the reduction of ACE2. The ACE2 protein specifically works to convert Ang II into Ang-(1-7) (Yuan et al., 2021). Ang II induces pro-inflammatory effects within lung tissue, while, Ang-(1-7) produces anti-inflammatory effects (Yuan et al., 2021). As SARS-CoV-2 uses ACE2 as an entry receptor of infection, it results in the decline of ACE2 protein function (Yuan et al., 2021). This decrease in ACE2 leads to enhanced and protracted tissues, and vessel exposure to Ang II, which then induces thrombosis, cell proliferation and recruitment, increases tissue permeability, and cytokine production–eventually inducing the deleterious inflammatory response (Yuan et al., 2021). The simultaneous destruction of alveolar walls from alveolar epithelial type two cells and the inflammatory response cause the alveoli to be destroyed and filled with fluid–effectively hindering the gas exchange process in the lungs.
Part three: Impact on the Respiratory System
The simultaneous destruction of alveolar walls from alveolar epithelial type two cells and the inflammatory response cause the alveoli to be destroyed and filled with fluid–effectively hindering the gas exchange process in the alveoli–leading to hypoxia (Yuan et al., 2021). Due to hypoxia developing in the alveoli, their ability to clear the edema fluid is hindered–partially due to the disassembly of the keratin intermediate filament network, which is a fundamental element of the cellular cytoskeleton (Yuan et al., 2021). This, thus, leads to more damage to the epithelial tissue barrier and results in the spread of pneumonia throughout the lungs. As the alveoli in the lungs deteriorate and fill with inflammatory material, the ventilation and perfusion rates within the body decrease dramatically. This results in the lack of oxygen being circulated throughout the body for use–effectively impeding all functioning.
References
Alipoor, S. D., Jamaati, H., Tabarsi, P., & Mortaz, E. (2020, November). Immunopathogenesis of pneumonia in COVID-19. Tanaffos. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7680509/
Covid-19 pneumonia: Symptoms, treatment & recovery. Cleveland Clinic. (2022, August 10). https://my.clevelandclinic.org/health/diseases/24002-covid-pneumonia
Mascolo, A., Scavone, C., Rafaniello, C., De Angelis, A., Urbanek, K., di Mauro, G., Cappetta, D., Berrino, L., Rossi, F., & Capuano, A. (2021, April 20). The role of renin-angiotensin-aldosterone system in the heart and lung: Focus on covid-19. Frontiers in pharmacology. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8093861/#:~:text=In%20the%20lung%2C%20the%20classic,(including%20COVID%2D19).
Yuan, S., Jiang, S.-C., Zhang, Z.-W., Fu, Y.-F., Hu, J., & Li, Z.-L. (2021, July 26). The Role of Alveolar Edema in COVID-19. Cells. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8391241/#:~:text=Since%20the%20exudation%20of%20pulmonary,and%20the%20blood%20oxygen%20content.

Nikolena Wulvik’s project was about the damaging effects of Covid-19 and how it can cause pneumonia in the lungs. In her project, she portrayed a pair of lungs, the right one being a healthy lung and the left being one with Covid-19. The objective she covered was, “Analyze the effects of disease on the function and structure of the respiratory system.” She made her project by molding clay into the shape and applying resin over it. In her paper she first discussed the Covid-19 infection that is part of the coronaviridae family, SARS-CoV-2. The virus is enveloped by the positive-strand RNA. The lungs are really susceptible to infection because it is an airborne disease so the droplets easily get into the lung tissue. Next discussed was pneumonia and the alveolar epithelial type two cells which are a defense mechanism get targeted by Covid-19 which leads to the surface area tensions causing cell death. The decrease of these cells causes the alveoli to collapse and become fluid filled, which is pneumonia. Finally, she talked about the impact on the respiratory system. Since the alveoli sacs are collapsed and fluid filled, they are unable to do gas exchange at the same rate they used to be able to, causing it to become pretty difficult to breath. The hypoxia caused from the pneumonia also causes more pneumonia to happen due to the damage of the epithelial tissue barrier. Very good project! I thought your artwork was very interesting and well done.