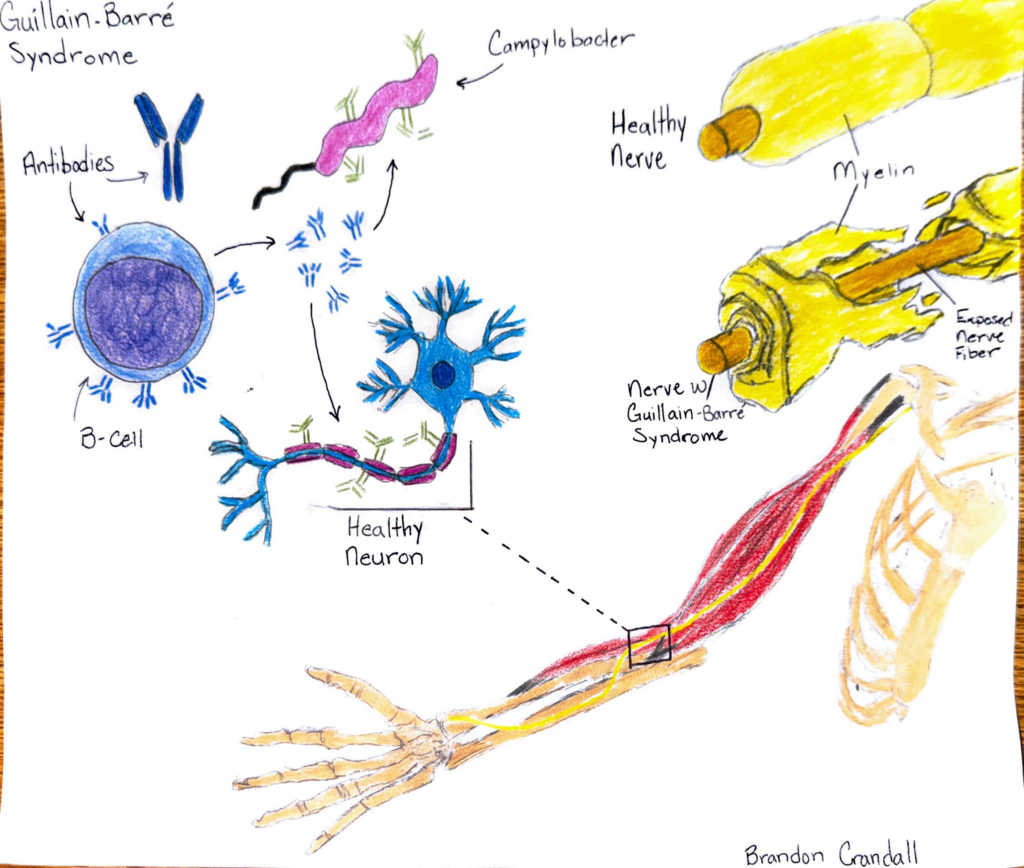
Guillain-Barre Syndrome (GBS) is a postinfection monophasic polyradiculoneuropathy. Meaning inflammation and demyelination of the peripheral nerves for one to three years and never happening again. While there is a chronic version of GBS, this can be either cured, or in severe cases, managed. Around five percent of patients with GBS pass away. Typically, GSB is not a disease that just develops within the body. It begins after an infection that the body has fought or is fighting off. The most common bacteria that causes GBS is campylobacter jejuni, however, many things can trigger GBS. The outer membrane of campylobacter jejuni contains lipo-oligosaccharide (LOS). LOS plays a major role in structural integrity of gram-negative bacteria and provides a protective barrier from external factors. When the body is exposed to campylobacter jejuni, the immune system gets to work by producing antibodies to attack the antigens on it. The LOS on the outer membrane of the bacteria triggers this immune system response. Lymphocytes, such as B-cells are responsible for producing the antibodies that attack campylobacter jejuni. Unfortunately, within both the LOS and the peripheral nerve gangliosides are some partially identical structures. Because of these similarities, the antibodies produced by the b-cells may not be able to tell the difference between campylobacter jejuni and myelin sheaths. One of twenty campylobacter jejuni infections leads to GBS. Antibodies are not alive, nor intelligent, so they are not able to use critical thinking when performing their duties. They are to simply park themselves within a receptor in which they fit. To the antibodies, there is no difference between campylobacter jejuni or nerve tissues. If it fits, they sits. This mishap is known as molecular mimicry. When these antibodies attack, the process of demyelination begins. Demyelination is the process of damaging or destroying the myelin sheaths that surround the nerve fibers. When there is a loss of myelin sheath, the transmission of electrical impulses throughout the nerves is disrupted. This can lead to many neurological symptoms such as weakness, sensory defects, areflexia, hyporeflexia, bulbar palsy, ataxia, etc.
While Guillain-Barre Syndrome is a serious and possibly deadly disease, it is also highly treatable. Treatment should be started as soon as possible if a provider determines it is necessary. This is because not only will it give better treatment outcomes, but the main mode of treatment becomes ineffective when neuropathic processes have resolved. In fact, the treatment therapies could be harmful if not performed in a timely manner. The two modes of treatment are intravenous immunoglobulin and plasma exchange. Neither have been found to have a higher or lower efficacy, however intravenous immunoglobulin is much easier to acquire and use than performing plasma exchange. The regimen for intravenous immunoglobulin includes 2 grams per kilogram of body weight dripping over five days. So, the average person would receive 160 grams over 120 hours. There are considerations for treating GBS based off severity of symptoms. If symptoms have presented for less than four weeks, some considerations include unaided walking, new or progressive respiratory distress, or dysphagia. Should the patient be unable to walk on their own, or show other previously listed signs, treatment should begin immediately. Should the patient complain of symptoms of weakness, or loss of neurological function lasting greater than four weeks, it is likely not GBS and a differential diagnosis should be considered.

Hey Brandon! I enjoyed learning about your STEAM project and here are the main insights I’ve learned from your project. Guillain-Barre Syndrome (GBS) is a rare but serious condition where the body’s immune system mistakenly attacks its own nerves. These instances usually happen after an infection which is mainly caused by the bacteria Campylobacter jejuni. The bacteria’s outer membrane contains lipo-oligosaccharide (LOS) which is a structure that looks similar to parts of the myelin sheath (the protective layer around the nerves). The immune system produces antibodies to fight off the infection however, these antibodies are not able to differentiate between the bacteria and the nerves myeline. This confusion also known as molecular mimicry, causes the immune system to attack the nerves, damaging their myelin and disrupting communication signals. This process is known as demyelination and causes symptoms like muscle weakness, loss of reflexes, trouble walking and sometimes difficulty breathing or swallowing. GBS does not cause a high percentage in death (5%) and is highly treatable if caught early. Some treatment options include intravenous immunoglobulin (IVIG) or plasma exchange, both of which can help stop the immune system from causing further damage. In these cases, quick and early treatment is crucial because delay in treatment could decrease the effectiveness. Your STEAM project nicely captures the journey of GBS, beginning from the initial infection to nerve damage. Additionally, it shows how Campylobacter jejuni triggers the immune response and how antibodies mistakenly attack healthy nerves. Your comparison of health and damaged nerves also displays the destructive process of demyelination, while the skeletal arm with exposed nerves displays the real world effects of GBS on the body.