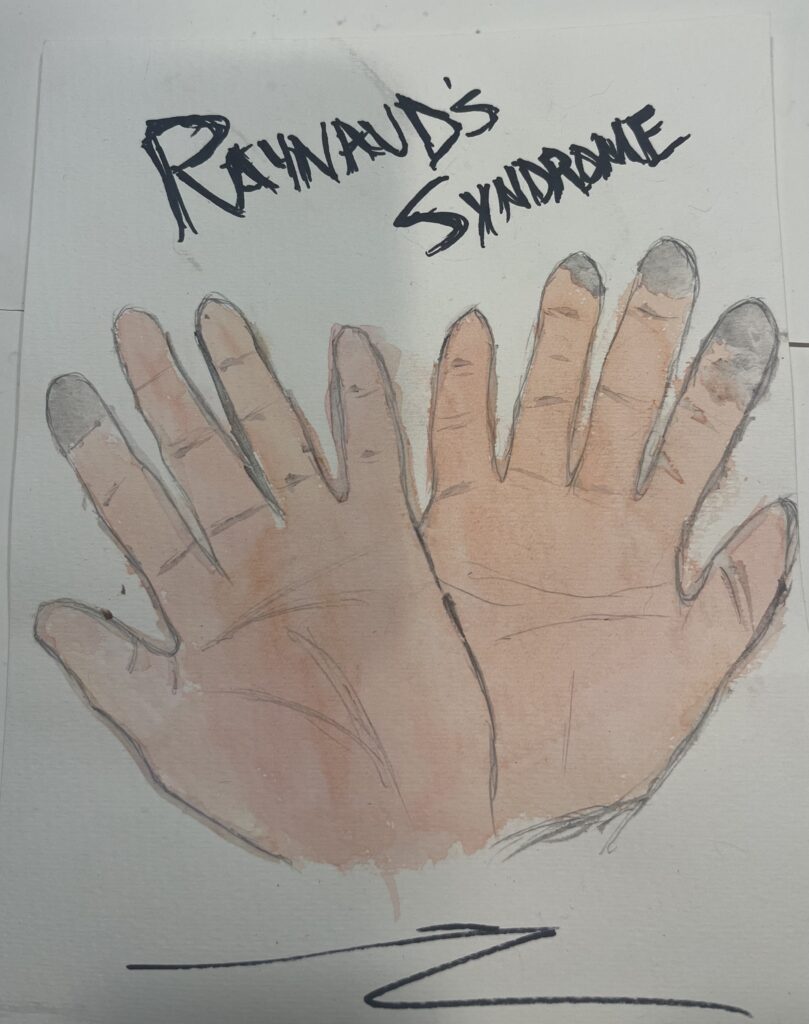
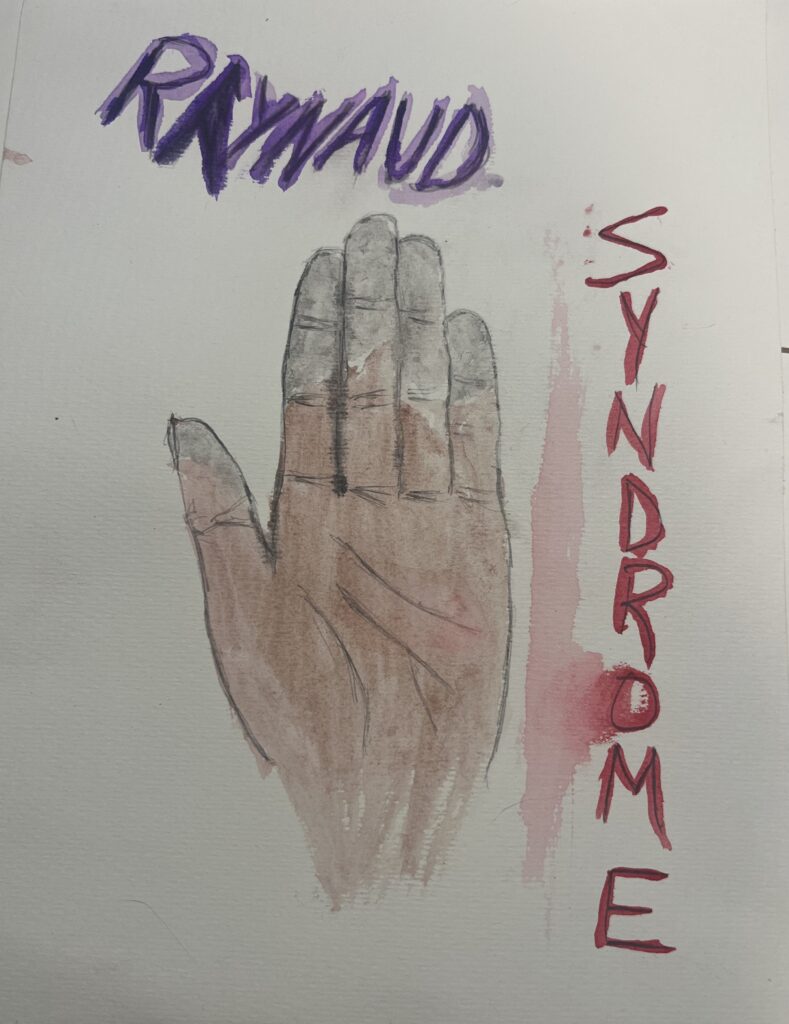
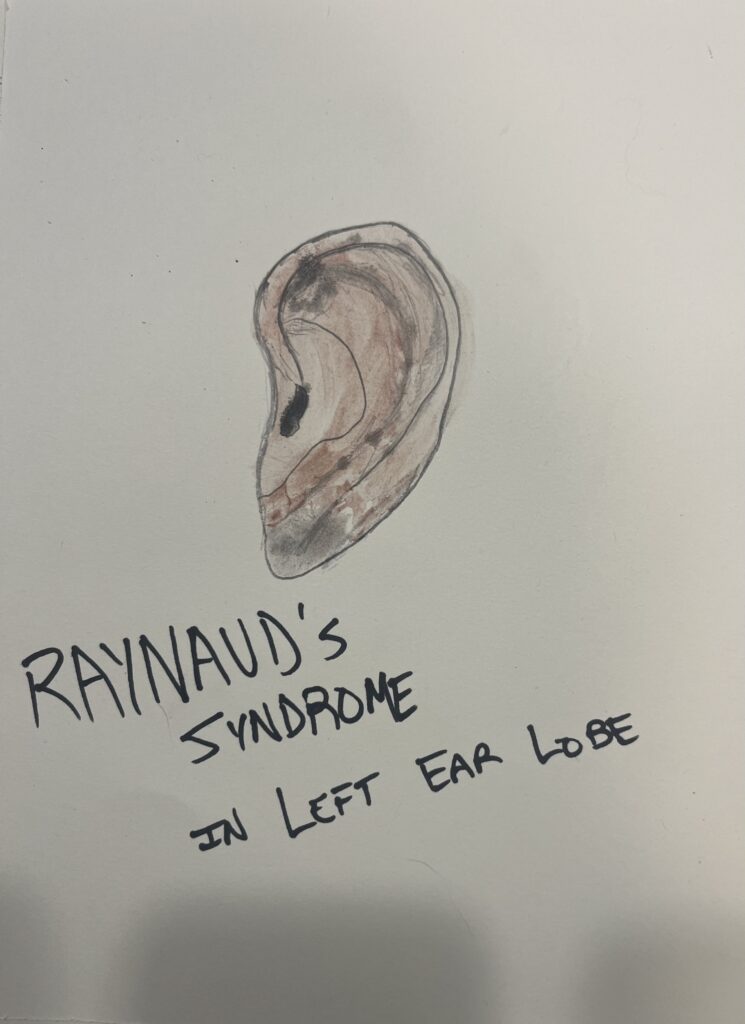
I chose to do my STEAM project on Raynaud’s Syndrome, also known as Raynaud’s Phenomenon or Raynaud’s Disease. I am tying it to the course objective of knowing the path of blood through the heart and the circulatory system. Raynaud’s syndrome affects the supply of blood to the fingers and toes, and it can also affect the nose and earlobes. My first image is a watercolor painting of mild scoliosis in the fingers. The second image I painted is a more extensive Raynaud’s that is affecting more of the fingers of a person’s hand. Finally, my third image depicts Raynaud’s on a person’s ear. As I depicted in my painting, typically, when affecting a person’s ear, it is localized to the earlobe itself.
Raynaud’s Syndrome is named after the physician Auguste Gabriel Maurice Raynaud, the first to describe the syndrome in his doctoral thesis from 1862. Raynaud’s Syndrome is typically characterized by vasospasms of the fingers and toes, often precipitated by exposure to cold. This exposure to cold often does not have to be extreme temperatures or below freezing. Mild cases of Raynaud’s are the most common; it is often idiopathic and not indicative of a more serious underlying condition. However, the first episodes of Raynaud’s can be rather startling or discomforting for patients. Often it triggers further assessment to rule out any possible underlying conditions. “The classical progression consists of triphasic color changes: well-demarcated pallor of the digits leading to cyanosis, pain, and numbness, followed by a red flush upon rewarming. However, typical episodes involve pallor followed by rubor, with cyanosis present only in severe disease. Early episodes might involve only a few fingers, but with time most fingers are affected.” (Block, J.A., & Sequeira, W, 2001. Raynaud’s Phenomenon.) Raynaud’s can progress to the toes, but it is often less pronounced in this area of the body because people are likelier to keep their feet inside their warm socks and shoes outdoors. Rarer cases of Raynaud’s can also be found on the earlobes and nose, presenting with white discoloration at the tip of the nose or earlobe. To an even lesser extent, Raynaud’s can be found in the nipples and tongue.
Raynaud’s is found in people all over the world but has a higher prevalence in cold climates where exposure to low ambient temperature is more likely. “Thus, the prevalence of the disorder in Charleston, SC, USA, and Barcelona, Spain, has been reported as 5·7% and 4·7% in women and 4·3% and 3·2% in men, respectively. Conversely, in Tarentaise, France, where the mean January temperature is −0·4°C, the prevalence is 20-1% in women and 13-5% in men; a similarly high prevalence has been reported in Denmark.” (Block, J.A., & Sequeira, W, 2001. Raynaud’s Phenomenon.)
Raynaud’s is classified as primary, which is idiopathic and has no know underlying illness or cause. The other classification is secondary, associated with another disorder after assessment. It is most frequently associated with Scleroderma, with 90% of patients experiencing Raynaud’s, followed by Lupus with 10-25%, Sjogren’s Syndrome with 20%, and Rheumatoid arthritis with 10-20%.
Treatment of Raynaud’s includes non-pharmaceutical measures such as avoiding cold temperatures, managing emotional stress, caffeine intake, smoking cessation, and avoiding vasoconstrictive medication. Pharmacologic measures have typically “included dihydropyridine calcium channel blockers, alpha1-adrenergic blockers, angiotensin II receptor antagonists, topical nitroglycerin, and pentoxifylline.” (Levien, T. L. (2010). Advances in the treatment of Raynaud’s phenomenon.) Further studies into vasodilators and topical nitroglycerin creams are showing improvement in treating symptoms of Raynaud’s. Raynaud’s continues to be evaluated and studied by researchers to identify causes, and treatments, and form a better understanding of the disease.
Block, J. A., & Sequeira, W. (2001). Raynaud’s phenomenon. The Lancet, 357(9273), 2042–2048. https://doi.org/10.1016/s0140-6736(00)05118-7
Levien, T. L. (2010). Advances in the treatment of Raynaud’s phenomenon. Vascular health and risk management, 167-177
Hughes, M., & Herrick, A. L. (2016). Raynaud’s phenomenon. Best Practice & Research Clinical Rheumatology, 30(1), 112-132.
Herrick, A. L., & Wigley, F. M. (2020). Raynaud’s phenomenon. Best Practice & Research Clinical Rheumatology, 34(1), 101474.