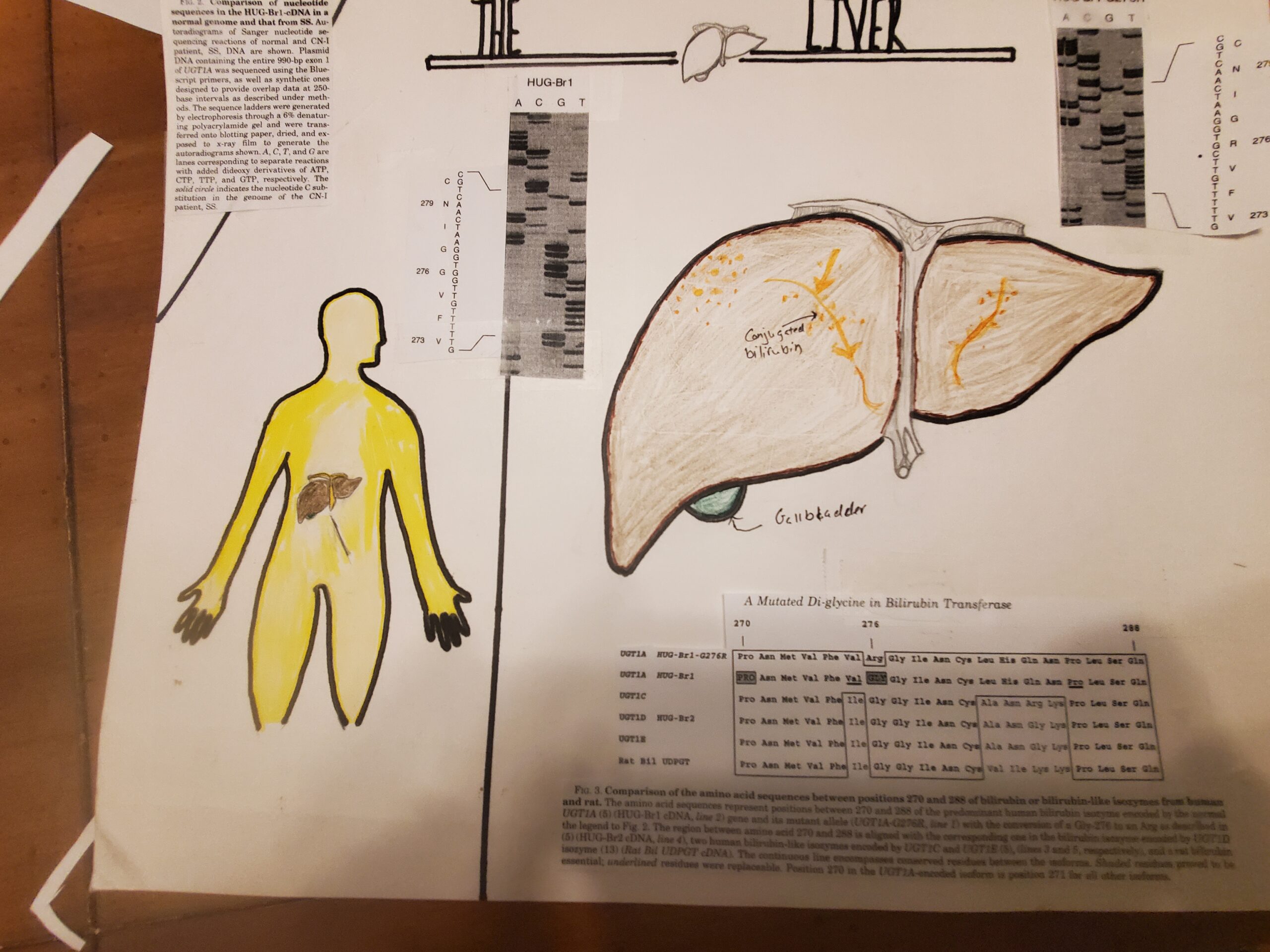
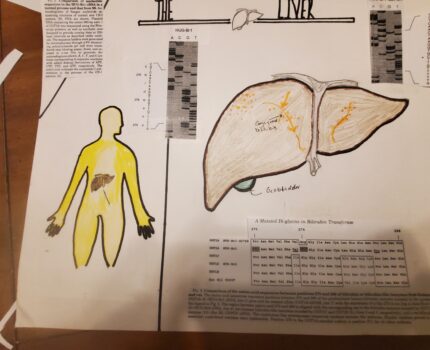
The liver has many functions to help the body, for example, remove waste by producing bile and break down fats in the small intestine during digestion. They can also produce certain proteins for blood plasma and can regulate blood clotting. Clearance of the bilirubin is another function of the liver can, removing bilirubin from the red blood cells. Cringler Najjar Syndrome is caused by an accumulation of bilirubin, which turns the skin and eyes yellow. For my art piece links to functions of the liver objective, I have asked my niece to draw a person and a liver. I wanted to show what happens to the skin if there is an accumulation of bilirubin. For the liver, I wanted to emphasize Crigler-Najjar’s abnormal state and what happens when one liver enzyme is not present. I would include different codes given to my parents regarding this disorder.
Crigler-Najjar syndrome is a rare genetic disorder in the liver that cannot properly convert and clear bilirubin from one’s body (Roy-Chowdhury,2016). There are two types of Crigler Najjar Syndrome. Crigler-Najjar syndrome type I, and the other is Crigler-Najjar syndrome type II or Arias syndrome. Crigler-Najjar was named after two doctors. Who discovered this syndrome? Dr. John Crigler and Dr. Victor Najjar back in 1952 when they noticed six infants whose parents were blood-related had this syndrome. In 1962 Dr. Arias discovered the milder version of the syndrome, which is now called Crigler-Najjar Syndrome type II. My main force will be on Type I, what causes this syndrome, and treatment for those who suffered from this rare syndrome.
Crigler- Najjar syndrome is a rare disease that affects 0.6 to 1 in 1 million newborns worldwide. Type I Crigler-Najjar is considered severe compared to Type II; type I is a disorder categorized for the absence or decreased activity of UDP-glucuronosyltransferase, an enzyme that requires glucronidation of the unconjugated bilirubin in the liver (Bhandari, Thada, and Yadav, 2021). For Cringler-Najjar syndrome type I, if the levels of conjugated bilirubin rise, this can lead to jaundice in newborns. The plasma compartment represents about 40mL/kg body weight, and in patients who have jaundice, the total equally is distributed between intravascular and extravascular (Strauss, Ahlfors, Soltys, Mazareigos, Young, Bowser, Fox, Squires, McKiernan, Brigatti, Puffenberger, Carson, &Vreman, 2019).
My older sister is a success story for hepatocyte transplant; in July 1988, she was barely seven at the University of Nebraska, received a new liver from a donor just in time. Since this was very new and only a paragraph about the disease, her survival rate was low; her Hepatologist expects her life expectancy was only up to eighteen, even with medicines and blood work that checks liver functions. Today is a mother and wife and past the suggested life expectancy.